As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
The post Sharing what works: 4 ingredients of our memory assessment service success appeared first on Here.
]]>Sharing what works: 4 ingredients of our memory assessment service success

I wrote an article for The Royal College of Psychiatrists regarding our memory assessment service and some of the ingredients that make this a service that delivers exceptional performance as well as compassionate, holistic care.
Can you ever really take learning from one place to another?
Many triumphs in one setting have been tried somewhere else only to meet disaster. We’re incredibly proud of what we – Here, a social enterprise with a mission to deliver exceptional care, for everyone – have achieved with our memory assessment service in Sussex. But if what we’ve learnt in Brighton and Hove can’t carry to Basingstoke and Bury, why should I even write this article?
A clue might be in a great paper by Mar Dixon-Woods and team about efforts to reproduce successful patient safety initiatives. “Without understanding the ingredients of success” the Health Foundation funded paper writes, “efforts to reproduce an improvement programme risk mimicking its superficial outer appearance, but not replicating the essential processes that actually make it work.”
So in an attempt at getting to those ingredients of success, here are four key learnings from our journey.
1. It’s more than a service
The B&H MAS is more than an assessment service. It is a community service delivered in partnership (Sussex Partnership Foundation Trust & The Carer’s Centre), providing clinical and support pathways that are fully integrated in one service. We are a lean team that is nurse lead assessment service supported by consultant psychiatrists and GPwER. All clinician work with our non-healthcare professional (support workers) and have a symbiotic relationship that supports personalised and holistic care.
It’s also a prime example of our organisational values and purpose and our commitment to both high performance and quality provision. Here delivers NHS services, across large and small geographical areas in Sussex while also providing business intelligence and transformation services across the NHS national system.
There is no one best model for memory assessment services but this model has delivered exceptional performance, outcomes and experience for patients, with results we are proud to share that have led to us achieving:
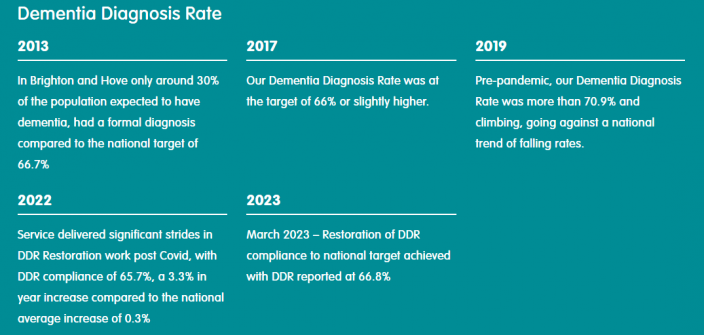
– DDR compliance both pre and post covid, significantly exceeding both the national target (66.7%) and the national and ICS average.
– Rated CQC Outstanding.
– MSNAP Accreditation Level 3.
– Letter of Commendation from MSNAP Board.
– Received MSNAP Sustainability Award.
– Exceptional Patient Satisfaction results >90% over last 5 years.
– 76% of patients reported maintaining or improving their quality of life (via the QOL-AD) within first year of receiving a dementia diagnosis.
Our success is all the more impressive given that the sustained transformation was delivered within the existing financial envelope, without additional investment by commissioners during 2017 to 2020.
2. We thought we were good, but not good enough
In 2012 Here designed and mobilised an integrated service – highly innovative for its time and perhaps even more so today. Between 2013 to 2016 the service delivered improvements in DDR of around 30% and improved patient journey times for Referral to Diagnosis with commissioner set targets of 10 weeks.
As the service continued to surge forward, attaining commissioned journey time targets, there was an increasing narrative that speed was not what all our patients wanted and needed.
We identified there was a gap between commissioned provision and what people required. This learning was painful as despite our best efforts and integrated model, we were not delivering what mattered most to our patients. Diagnosis had been our priority and it was clear that our patients wanted a service that was designed around their priorities and needs, whilst giving them time and support to adjust to the possibility of receiving a diagnosis of a life limiting degenerative disease.
Putting aside our service specification, KPI and system rules we started a process putting our citizens at the heart of our enquiry.
We asked our patients key questions: what was important to them and what mattered most.
Over a 4-month period we conducted a System Thinking enquiry to better understand the needs and experience of the people who used our service. System Thinking analysis requires taking a step back, to investigate whilst looking at the wider picture through a more holistic lens to gain further understanding. Services do not operate in isolation, our healthcare system and the people we serve are complex and multifaceted and our investigation had to acknowledge this.
We also undertook case studies, direct observations, hosted patient and carer focus groups and reviewed the patient journey from referral to discharge. This accounted for approximately 15% of our caseload.
Our key learning was: Of the patients reviewed 70% that were requesting support, diagnosis was not their priority.
In 2017 with the consent of our commissioners, we redesigned our service around patient voice and needs and anchored ourselves to a new purpose created out of the learning from our patients and their loved ones:
To help me and my loved ones to get the care we need to live our lives well.
Our aim was to become a more compassionate and personalised service. Reallocating support from our post diagnostic pathway, we offered support at the point of referral to all, working proactively to meet patients’ needs. Our Dementia Advisors were renamed Memory Support Workers (MSW) and each patient was provided a named worker that held patient care. Our team built relationships with patients and their support network, ensuring everyone had ‘what mattered’ conversations at the start of their journey, whilst supporting people to navigate and integrate across the system.
3. It’s always about the patient journey
Adding another step to the pathway may seem counterintuitive as it could have extended or delayed patient journey times. However, this addition improved patient journeys and therefore ensured we understood our patients needs and support any barriers they might encounter whilst travelling through the service. Our MSW counselled people, listening to their concerns and explained how they would be supported if a diagnosis was made. Understandably for many the fear of a diagnosis was a barrier and the thought of clinical assessment and its outcome was something to fear and avoid.
4. We’re excited about the future and the potential of biomarkers
The redesign also taught us that there was significant unmet need in people who receive an MCI diagnosis. Given the inequity of biomarker via CSF, Here in 2022 expanded and delivered a pathway enhancement with our local trust UHSx, to create a dedicated biomarker pathway funded by Roche Pharmaceuticals. During 2022-23 we also attained our long-term goal of being commissioned as a lifelong service that aligned with commissioner intentions providing annual care planning and access to our established post diagnostic service.
So did I manage to convey some of the ingredients of our success? We’d love to know what resonated with you, and we’re always keen to learn from others.
Want to learn more?
To learn more about the B&H MAS visit our website or contact Jason via email (Jason.willcox@NHS.net).
Jason Willcox is Head of Dementia Provision with Here, Care Unbound Ltd. Jason is a Subject Matter Expert and has supported NHSE Improvement workstreams. He recently presented at NHSE national webinar sharing his learning from the B&H MAS as an example of high performing, high quality, holistic and personalised service.
Learn more here.

Also of interest
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Sharing what works: 4 ingredients of our memory assessment service success appeared first on Here.
]]>

