As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
The post Rethinking Our Health: starting with pain appeared first on Here.
]]>Rethinking Our Health: starting with pain
Our latest update from Jo Crease, Programme Manager at Here, shares our progress on Rethinking Our Health, a community-led approach to improving support for people living with long term conditions.
Picking up from the co-design sessions at the start of summer, Jo explains where we’ve got to since then, what we’ve learned from communities about MSK pain, and what we’re going to test next.
Rethinking Our Health – so, what are we actually going to do?
Over the summer, people have quite reasonably been asking what Rethinking Our Health is actually going to look like in practice. What are we going to do, where, and with who?
I’ve spent much of the last six months saying: “We don’t know yet, because we haven’t asked the community yet – and that’s the whole point!”
Now we’re at a point where we have asked the community, and this is what happened next.
A reminder: what is Rethinking Our Health?
Rethinking Our Health is our shared programme with The King’s Fund to explore new ways of supporting people with long term conditions, starting from what communities say matters most.
How we’ve been working with communities and VCSE partners
Over the past few months, we’ve been in rooms with community members, VCSE organisations and partners, testing ideas together and challenging our own assumptions – rather than deciding solutions from the centre. After these sessions, all the collaborators came together to make sense of what we’d heard, compare insights and pull the learning into one shared picture.
Why we chose to start with pain
We all agreed we wanted to improve support for people with long term conditions – and we chose to start with “pain” as a way to talk with and support people who were struggling to get what they need.
But the priorities weren’t always the same.
Here and The King’s Fund were thinking about the longer-term challenges in how health and care needs to work in future. Our test site partners were focused on the immediate reality of people not being able to get what they need right now.
Once we recognised that difference, the question became: how do we create something that works for both?
We tried to square that circle by starting from the community’s point of view and seeing how that could lead towards more sustainable solutions for the NHS.

What we learnt from truly listening to communities
As we tested ideas locally, a pattern emerged.
In spite of our best intentions, we were still coming across as “here’s something we’ve designed for you”, rather than “here’s how we want to build with you, starting from where you are right now”.
There was also a clear expectation that anything we offer had to genuinely solve problems people already face and not feel like yet another ask for people with busy lives and services that are already stretched.
We also learnt that creating new roles, like ‘Champions’, wouldn’t be welcome. People are already active in their communities, with their own motivations and networks. They don’t necessarily want another label or obligation – especially one created by public services rather than driven by what actually matters locally.
Community development organisations work because they start with what people already have: their strengths, motivations and contributions. They don’t impose new ones.
This feedback was honest and challenging, but it came from trust. We’ve worked hard to build that trust over the last six months, and because of that, partners were able to give this critique, and we were able to hear it – and act on it. And we know the work is stronger because of it.
Our response: a three-part community offer on early pain
People told us they wanted:
- Trusted advice, early enough, local and accessible
- A way to understand more about MSK pain
- People working in the community being part of a solution together
Working with our test sites, we’ve refined the goal to build neighbourhood-level awareness, capacity and confidence to act on early pain. And we’re doing this through three interlinked elements that are, crucially, built on existing community assets and relationships.
1) Trusted advice, early enough, local and accessible
Community Health Drop-In
A weekly half-day drop-in hosted by a Community Development Worker, with a physio and a social prescriber. This is a space for advice, guidance, support with social factors and community connection.
2) A way to understand more about MSK pain
Community learning and peer support
Four modules covering: pain management, medication, exercise and movement, and general health and wellbeing. We are using a train-the-trainer model so community workers can deliver these sessions in the longer term.
3) People working in the community being part of a solution together
Workforce learning offer
A CPD-accredited short training offer for people working in the community – primary care, VCSE, social care, libraries, food banks and volunteers – building confidence around early pain and health coaching and encouraging neighbourhood networks around pain.
What happens next
It’s still very much a work in progress – we need better names for the elements of the offer for a start (drop a comment with suggestions!).
We’re going live mid-November and running through to March in the first instance. The next update will share reflections from the first Community Health Drop-In. I’ll also be talking about how we plan to balance getting the data we need without overloading participants, and how we’ll involve community researchers in understanding people’s experiences of this work more deeply.
As always, let us know what you think – what questions do you have?
Drop us a line at collab@hereweare.org.uk
Want to follow the journey?
Sign up to updates direct to your inbox
Also of interest
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Rethinking Our Health: starting with pain appeared first on Here.
]]>The post Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust appeared first on Here.
]]>Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust

Reflections from our first Rethinking Our Health codesign workshops.
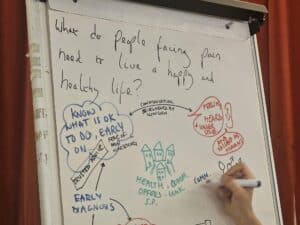
Codesign events with communities and partners
July saw an important milestone in Rethinking Our Health, with our test site partners we held community codesign events to share back the findings of the engagement phase, and to discuss practical ideas to take forward in the autumn. These will be focused on our goal of community-designed, clinically backed support for people with or at risk of osteo-arthritis, cardiovascular disease and diabetes.
A mix of lived and professional experience

At both events we had a half and half mixture of community members and people who work in health, local government, and the voluntary community and social enterprise (VCSE) sector.
Designing the events with the community
Both events were planned with our test site partners and community members, and this is key to how they went. This meant focusing on the biggest things people told us about in the engagement phase – there were pain, access to services, understanding and confidence around your condition, practical social and financial barriers.
Two areas, two approaches
In one test site there has been a history of (and a funded infrastructure for) conversations and partnership working. Over the last ten years, many issues have been discussed, the progress both desired and created by all, the codesign event felt natural. It felt like we could ask things of each other.
In our other area leadership is more dispersed, local government takes a bigger role in leading and encouraging community health and engagement partnership working. Test site partners took a participatory appraisal approach to developing community engagement in our big question, and the pre-event work was important to building interest and confidence to take part.
Shared energy and commitment
One thing in common was that both events were buzzing with enthusiasm and commitment to neighbourhoods was clear. There is a real appetite for building on existing or previous work, ambition for better solutions and understanding that so much of this is built on relationships.

What we heard: Key themes from the codesigns
Key themes that came out of both events were
- desire for local, early, holistic support
- positive and ambitious views on the role of community and VCSE in this
- community engagement and mobilisation, patient leadership and voice is critical
- importance of being heard, and *feeling* heard – both in individual situations as well as a community
We heard a range of views about what kind of support could be given by clinicians versus non-clinicians, and creating different configurations of how community and clinician support could be offered together.
Clinical risk and collaboration
There’s an important discussion to be had about understanding and managing any clinical risk, which Here as a clinical and community-rooted organisation is well-placed to host.
Looking ahead

This way of working is how health care will be developed over the next ten years and beyond.
Dr Rowan

For now, sign up to receive an update when we publish the next blog. Want to get in touch about Rethinking Our Health? Email us: Collab@HereWeAre.org
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust appeared first on Here.
]]>The post How do we build personalised care into our services? appeared first on Here.
]]>How do we build personalised care into our services?

How does our Memory Assessment Service provide personalised care that makes a real difference to people?
In my first week at Here, I was sharing space with the Brighton and Hove Memory Assessment Team. I was privileged to hear one side of a conversation between one of our Memory Support Workers (MSW) and a person who was accessing the service for the first time.

Can you say a bit about how personalised care is the foundation of the MAS?
Our Memory Assessment Service purpose is “To help me and my loved one get the care I need, to live my life well”. We designed the service around the understanding that everyone is different with different needs, but they also have strengths and assets. Having a memory assessment can be scary, we wanted to acknowledge this and think about how we provide our support to be built around people with the aim of offering the best experience for them.

How do we apply those principles in practice? What does it practically mean in developing and running the service?
The main difference with the way we work is that we offer wrap-around support from a named Memory Support Worker (MSW) from the first contact call to assessment and care planning. That first contact call is really important. It’s a chance to build a relationship with someone. Our first contact call template is designed based on What Matters To You (WMTY) principles.
We ask the person about what they’re experiencing, what’s important to them, and who is important to them.
This lets us offer support based on their strengths and needs, for example, are they struggling with personal care or food, getting out of the house. These things can affect someone’s general health as well as their memory, and support offered at this point can really help people while they’re waiting for their assessment.
‘What’s important to you’ helps us understand what a priority for them in terms of diagnosis, treatment and support options. And ‘Who is important to you’ helps us to understand their support network and identify if they may be isolated and need extra outreach, or if families and loved ones need support also.
People get a letter with the details of their named MSW who will be with them throughout, and when they have their appointments with the clinician, the clinician will have access to the records from the MSW and vice versa, so it is seamless for the person.
If they do have a diagnosis, they then have a Care Planning appointment with their named MSW, who they will have known since the beginning, and the relationship they have built up helps create a really tailored care plan.
What roles do we have and how are they different? How do we train and support staff in MSW roles?
We developed our Memory Support Worker role to provide the pre and post diagnosis support and to be that named person all the way through.
When MSWs join us, they have a programme of shadowing across all the other roles in the service, from admin team to clinicians. They experience assessments and diagnosis appointments, and MDT (how the diagnosis is formulated). Then they shadow experienced MSW to learn about the different call types and how the templates guide you through. They see some of the scenarios that they might experience in their new role.
They learn about communication styles and how would you alter your communication style depending on the person and what they need.
They then have Guided Practice with an experienced MSW to either help during the call, or to feedback afterwards. This is helped by our technology allowing three-way calls. All MSWs have monthly 1-1 supervision and monthly group supervision with other MSW.
Group supervision is an opportunity to discuss cases, share learning and support each other, and to think about potential changes that we can make to improve the service.

Are data and case management systems structured any differently to facilitate the WMTY approach?
We use SystmOne (S1) and the data and analytics team at Here are experts in design and use of S1 in clinical services and this has allowed us to build and continually evolve our templates in S1. As all staff are S1 users, all the relevant information about people we work with is accessible to everyone in the team.
Each appointment type has its own template which we’ve created and adapted as we’ve developed as a service. For example, with the First Contact Call template we have added in fields for demographics and reasonable adjustments to make sure we’re thinking about what the person might need, and offering adjustments such as the type of information they need or help getting to appointment, if someone’s religion means they need appointments on certain days, or if they have a preference for the gender of their clinician, and what their interpreting needs are.
On a service level we use PowerBI for reporting on deliverables and KPIs, but we also do additional analysis and add that to knowledge gathered through patient experience. This can help identify and address gaps, for example, we did some analysis by demographics and identified that the service possibly wasn’t meeting the needs of our LGBTQ+ patients.
We approached Switchboard Brighton & Hove LGBT Switchboard about collaborating together to understand better the needs of the local LGBTQ+ community. As a result of this learning, we then made changes to the language we used, it influenced our collection of demographic data by placing more importance on this group to help us provide more personalised care and support and in signposting/referring people to the most appropriate services for them. This is a start, and we want to carry on listening and improving our service in this way.
What challenges can it throw up, if any?
Everyone will be aware of the pressures that health and care, and voluntary sector organisations are under, and this does affect what we’re able to do. We try to be as proactive as possible, but there may not be capacity in the wider system to respond to this.
In terms of running the service, there is a risk of an emotional toll on staff because of the engagement with individuals that we offer. Helping our team to learn how to manage the impact on themselves of this work is key and I mentioned above the importance we place on 1-1 supervision and group supervision, which is really important for that emotional side of things as well as the professional or practical.
We also encourage informal peer support such as team chats, colleagues giving each other opportunities to debrief after difficult calls, and support from managers to take time to process situations if needed. In terms of leadership and always seeking to grow our practice, and develop our service, the NHS Sussex Personalised Care Network is a way to connect with others locally who are doing similar work.

What would be your recommendation for others starting on this journey?
In terms of developing a service in this way, it’s important to listen to the people using the service and take on board their thoughts and feelings.
When working with individuals, the key is really active listening and being purposeful about what recommendations or support offered, not offering all the things on the list, but focusing on one step at a time and going at the person’s pace.
Leadership in your organisation is key too, they have to really get and be committed to personalised care.
It’s the stories that bring it to life, showing the impact that you can have by working in this way.
When I worked as an MSW, I visited a person who was very isolated, couldn’t cook for himself, couldn’t get out because of steps up to his front door. We worked closely with Ageing Well service in Brighton & Hove, and they helped him with cooking, shopping, lunch clubs and then ultimately with a move into supported accommodation. He has a mobility scooter now and goes out nearly every day. He’s in a much better place.
Listening to what he wanted and what he was missing out on has had a massive impact on his quality of life and therefore on his condition.
I think it’s important to remember that people are not just their health condition, and that their wider social situation can have such a huge impact on their health and wellbeing.
Dementia is progressive, so it’s essential to focus on quality of life.
People can still live well, and it’s so rewarding to be able to help that happen.
The Sussex Personalised Care Network aims to:
- Improve workforce knowledge, skills and confidence in personalised care.
- Connect staff across the Sussex to create opportunities to grow, learn and lead on personalised care together.
- Share experience, resources and practical solutions to challenges.
- Demonstrate impact of Personalised Care for people, workforce and system.

Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post How do we build personalised care into our services? appeared first on Here.
]]>

