Back in 2016 we redesigned the Memory Assessment Service (MAS) following feedback from the people that utilise it. They told us that they believed diagnosis was not as important as support.
Here is the story of Paula, one of the MAS service users. We take a look at Paula’s life with her family before, during and after being supported by the Memory Assessment Service. Names have been changed to protected identity.
Paula’s Background
When Paula was first put in touch with the Memory Assessment Service (MAS) she was 75 and lived alone. She had always been proudly independent having been a working, single parent, has a great sense of fun and an adventurous streak.
Paula had a close relationship with her daughter who lives abroad, but did not have any local family that she was close with. Paula had recently been diagnosed with vascular dementia and was struggling to come to terms with this, expressing some suicidal thoughts. She can be particular about her support, her home, and the people she mixes with. For this reason it has been difficult to introduce support like befriending services or lunch clubs.
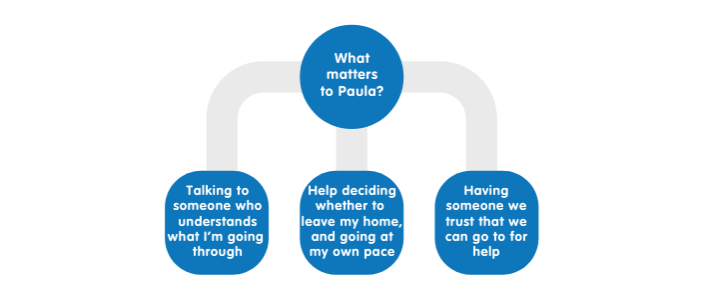
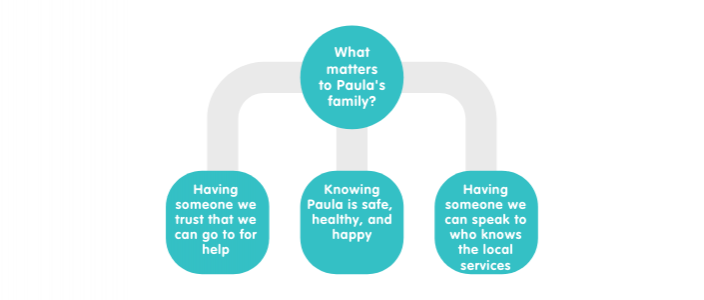
Understanding what’s important to everyone
The practical support that Paula received from MAS
Paula wanted to move into sheltered housing but was nervous about leaving her home, and wants the place to be right for her. Her Memory Support Worker (MSW) listened to Paula’s wishes and after a year of discussions, referred her to ‘extra care’ housing scheme for people with dementia. The MSW arranged a social care assessment in order for Paula to be considered for the housing scheme
Although Paula was independent she felt lonely, so the MSW gave lots of information, referred her on to services and offered to accompany Paula to her first outing as she was nervous about this.
At the time, Paula’s family had concerns about her weight loss so the MSW discussed ‘meals on wheels’ with Paula and arranged for the manager to visit Paula at home.
Paula wanted to feel reassured when at home and the MSW arranged to be present for when Carelink visited.
Emotional support
The MSW helped Paula come to terms with her diagnosis, and reassured her that she is not to blame. As a result Paula has ‘opened up’ to her MSW and told her things in confidence. She calls them in times of need, and when she feels suicidal.
Paula’s family and friends contacted the MSW when they had concerns about her wellbeing and mental health. Her family were updated with any information or incidents about Paula’s care and were present for the transition over to Specialist Older Adults Mental Health Services.
Memory Assessment Principles
- We pay attention to your emotional and psychological needs
- We will hold you until we have found or helped you to find solutions to what matters to you
- You will help those you love/care for to support you
- You set the pace and end point and you will always know where you are in our service
Without the Memory Assessment Service
- Paula would have only received one initial visit, and two follow ups, and for only the 12 months following her diagnosis. After this she would have been discharged. With only this small amount of input it is unlikely that she would have built a trusting relationship with her MSW.
- Paula would have been discharged 12 months after her diagnosis meaning the MSW would not have been able to be involved in the transition to the specialist team
- Without this relationship, Paula may not have known who to contact in times where she felt suicidal. This could have led to a crisis situation and potentially harm or death.
- Paula was very resistive to any outside support e.g. befrienders, Carelink and meals on wheels. Without the support of her MSW she may never have accepted these which could have led to further harm through isolation, falls with no way to get help, and a deterioration of physical health due to weight loss.
- It is likely that without the input of the MSW, Paula would have needed urgent input either through hospital admission or respite and would not have been able to make her own choice about where she would stay.
“I would really like to tell you that I feel you really understand perfectly the situation and where mum is at the moment, I couldn’t describe it better myself! You are making such a difference, thank you.”
Outcomes for Paula
The MSW visited or called Paula over 20 times during her 17 months within the service. Paula now has Carelink at home which she feels reassured by as she can press it if she has a fall at home.
She also accepted ‘meals on wheels’ which she says she enjoys and is helping increase her weight. Paula has been accepted into the ‘extra care’ housing scheme and has been offered a flat on the top floor which she is happy about.
Paula is still experiencing varied moods and sometimes feels as though she can’t go on. She has expressed some suicidal ideation which requires more specialist input than what the MSWs can offer. Paula contacted her MSW in these moments, and the MSW referred her onto specialist mental health team who are providing ongoing emotional and psychological support to Paula.
It was agreed that MAS should discharge Paula and let the specialist team take the lead. Her MSW helped Paula with this transition and provided useful information to the service so they can support Paula in a way that suits her needs and wishes.
No Comments
You may also like

22.07.2020 | by Lesley Jay
Hello Lesley Jay - Our New Finance Director
07.05.2020 | by Helen Curr
Hello Helen Curr - Our New CEO

04.08.2020 | by Matthew Riley
Hello Matthew Riley - Our Chief Information Officer and Head of CSI
