We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
A clinical view of the Stroke Health and Wellbeing Service Pilot: From Patient to Person

Consultant stroke physician, Dr Ingrid Kane, reflects on provisions for stroke survivors, and how the Stroke and Wellbeing Pilot has improved the lives of patients in Sussex.
If we go back to the first Stroke and Wellbeing Service meeting we had together – which was a long, long time ago in a hall in Brighton, it felt like it was a moment of change actually being at that meeting – because you had so many people from the community, from the hospital, everyone was there explaining how they are part of this system.
In all the time I’ve been doing stroke, I’ve never had the opportunity to be in a room with all those different people who were all involved in the Stroke and Wellbeing Service, and for us all to chat and listen to people and listen to patients, and there are so many people doing so many good things – it’s just not all joined up.
I’m involved in the care of stroke patients from when they come in to the front door, right until they leave the hospital and on into outpatients and following them up in clinic. As a workforce, we’re a big team, we’re a busy team, and we’re all trying to do different things and there’s never enough time. We don’t have enough staff to do all the work that we would like to do and that we should do.
If you speak to anyone at any meeting I go to, the one thing that is always an issue is people having someone that they can contact – that they know – to reduce that feeling of abandonment when they’re discharged from hospital.
To the patients who’ve been involved, it has made such a difference, in the feedback that we’ve had from those patients or relatives, even if it’s a casual comment as they leave hospital.

The Stroke and Wellbeing Service has really made an impact and it’s something that I would love to see continued because it’s made such a difference to people.
I think by having these other roles, it means that it frees up a bit of our time to be able to maybe concentrate on other things and let those other conversations that need time. let them happen through a single point of contact. I know when I have the time to spend more time with patients and their relatives, they get a lot out of that – one size doesn’t fit all.
It’s so difficult knowing how, for that individual, they can best navigate the system. And you only get to know that by getting to know people a bit better and having the time with them.
And you might try one thing that doesn’t work, then you move on to something else. If you’ve got the time to do that, that’s what makes all the difference.

When we get reports of people saying they feel abandoned when they go home, that’s not unique to Sussex, that’s wherever you happen to have your stroke. So I think the people that have been part of the system, the single point of contact with a stroke support worker is important. It can be used anywhere, it can be transferred to anywhere in the stroke system. And similarly, the health builders I think they are so important within the hospital, but also in the community as well.
The stroke pathway doesn’t stop when people leave here. It continues all into the community and it can continue for many months. And that was one of the things that we talked about when we first met is how do we get that true integration from acute into community and how can we get it to continue. Health builders, you just need more of them and more of those groups, and that could again apply to anywhere in the country and to any types of community groups, any age. All of these roles could be moved into other systems.
GP and clinical lead for the Memory Assessment Service (MAS), Dr Rachel Duncan, speaks about stroke research and the particular challenges stroke survivors experience.
There isn’t really a proactive offer from primary care to stroke survivors. So really, the ball is in the court of the stroke survivor to contact primary care with a particular problem. But we also know that this can be challenging because of capacity issues and difficulties with access. And you’ve also got a group of people who have cognitive, mood and energy problems, often in that time after they’ve had their stroke.
So all those factors make it a challenge for them, possibly to engage a lot with primary care. We know there’s a gap, we feel that we should somehow be doing more, but we don’t really know what that more looks like or how you could even provide that in the current healthcare arena when everybody is so pressured, and services are struggling to meet the needs.
Looking at what had been done locally, nationally and internationally, I came across a study called the IPCAs study, a really large study that was mostly funded by the National Institute for Health Research and was a collaboration with the University of Cambridge.
Their findings and our findings really mirrored each other. Yes, this is a local issue, but it’s also a national issue. It’s being identified, and what solutions could we find that might meet the needs of the patient and the system in order to rectify any gaps.

Out of those early discussions out of the case studies and the service mapping and identification of any gaps locally, came the idea of a stroke support worker, and the idea that people who’ve had lived experience have got so much to offer somebody who’s going through this sudden new diagnosis. A solution that isn’t completely clinically focused, but that meets those needs, to me, would make a lot of sense from a health economic point of view.
I’ve seen first-hand what difference it can make to patients coming through the service to have that support element embedded within our clinical team and how personalised and holistic that can be. Having that kind of support service really is of huge benefit to clinicians as well, because it does spare a lot of clinician time.
I think the fact that our local findings and learning really were mirrored by this larger study, the IPCAs study that I mentioned before, I think that’s got to be very powerful to hopefully, in the future, take this forward and have these kind of roles embedded across lots of different chronic illnesses. But I think stroke’s a good place to start.
Also of interest
Rethinking Our Health: Why it matters
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.
Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.
The post A clinical view of the Stroke Health and Wellbeing Service Pilot: From Patient to Person appeared first on Here.
]]>The post Expanding our Data and BI impact: How you can help us appeared first on Here.
]]>Expanding our Data and BI impact: How you can help us

We do Data and Business Intelligence (BI) well. Award winningly well in fact – but we don’t want to keep our knowledge to ourselves!
Over the years we have supported other healthcare providers on their journey. As well as our own services – we now want to expand our impact by partnering with more organisations to improve their Data and BI.
We want to understand what other providers, non-profits and Community Interest Companies (CICs) feel they need and why. To help us shape an offering that adds the most value, and truly does help other healthcare providers improve their own impact in care.
We are looking to talk to healthcare organisations, non-profits and CICs who:
- Are considering or planning their data and BI approach as a business need and have not fully embraced or realised good capability in this area.
- Are looking to mobilise or create a new clinical service enabled by the right data, analytics, and reporting.
- Are looking to improve or transform an existing clinical service or services, enabled by the right data, analytics, and reporting.

This market research will involve a 1-hour interview with our external researchers.
Ideally, we would be interested in interviewing those who are responsible for this work, or who oversee the strategy for your digital and data.
As a thank you to those organisations who are happy to participate. The Here Data and BI team would be very happy to offer an advisory hour on your Data and BI approach.
If you’re interested – we would love to hear from you!
Please contact matthew.riley@nhs.net for more in information.
Know someone else who would like to help? Share this blog with anyone you think might be interested.
You can also learn more about how our Data and Analytics helps us to provide exceptional care in our latest Impact Report.
The post Expanding our Data and BI impact: How you can help us appeared first on Here.
]]>The post Here launches Impact Report for 2023-2024 appeared first on Here.
]]>Here launches Impact Report for 2023-2024

Our Impact Report 2023-2024 is now up on our website, showing the impact we have and showcasing some of the great work we’ve been so proud of this year!
In our report you’ll find out about:
- How our Health Builders are a vital part of our unique person-centred approach.
- Celebrate 10 incredible years of MSK transformation with us.
- Learn about how our equality dashboards are helping us to find those who are not accessing health services and how we’re using the data they collect to co-create services that are better suited and accessible, for everyone.

Crawley Community Action’s Health Expo Event

Monopause@Work breakfast launch event
We would love you to hear your thoughts and feedback. Please feel free to share with anyone else you might think would like to find out more about us.
If you’re interested in working with us, or finding out more about our projects, partnerships and opportunities, please do get in touch. We love to connect, share best practice and explore collaborations.

The post Here launches Impact Report for 2023-2024 appeared first on Here.
]]>The post The CSP shares experience of Community Appointment Day in HSJ appeared first on Here.
]]>The CSP shares experience of Community Appointment Day in HSJ

We were lucky enough to welcome some of the team from The Chartered Society of Physiotherapy at our most recent Community Appointment Day to experience what this innovative approach is all about!
Sara Hazzard (She/her), Senior Strategic Communications, Campaigns, Policy, Improvement and Marketing Leader at The CSP has shared her thoughts about the day in a fantastic article for the Health Service Journal – ‘How to radically reduce your MSK waiting list in two days’.
The model allows clinicians to provide better care by working with local community services, focusing on prevention and health promotion, and truly reaching the people who really need this support.
You can read it in full here: https://www.hsj.co.uk/comment/how-to-radically-reduce-your-msk-waiting-list-in-two-days/7035793.article
Thank you to Sara, Mindy Dalloway and Clare Aldridge from The CSP for joining us.
To learn more about CADs: Community Appointment Days – An idea that rapidly turned into an innovation
Interested in learning more about how you could adopt the same approach in your local area? Get in touch:
Email: collab@hereweare.org.uk
Get in touch
Interested in learning more about our services, programmes and innovations? Fill out the form and we’ll get in touch.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post The CSP shares experience of Community Appointment Day in HSJ appeared first on Here.
]]>The post Those who dare: Exceptional care through an ‘everyone’ culture appeared first on Here.
]]>Those who dare: Exceptional care through an ‘everyone’ culture

Earlier this month our Head of People, Una Nicholson spoke as part of the – Those who dare: thinking differently about the health and care workforce conference held by The Kings Fund.
24 speakers contributed to the conference. They showcased projects and case studies aimed at encouraging others to explore innovative and positively disruptive approaches to meeting challenges facing the health and social care workforce. Including discussions about recruitment, retention, wellbeing, and equity, diversity and inclusion.
I was absolutely delighted to take part in a fascinating conversation about supportive and positive working environments and cultures with and for the people who deliver care across the UK. It was great to meet Catherine and Kerry and to hear about their ground breaking work. Thank you to The Kings Fund for this opportunity.
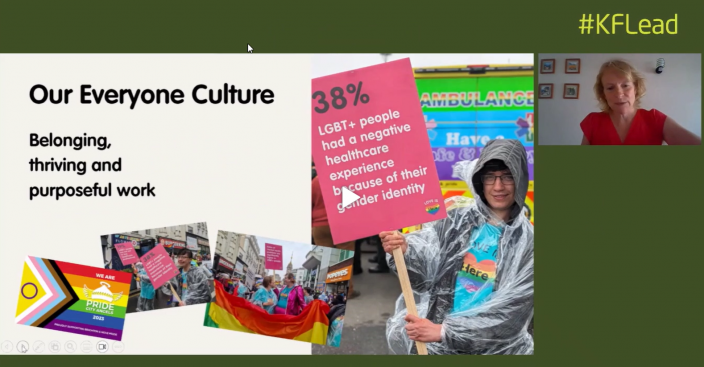
During Una’s session as part of the ‘workforce health and wellbeing and developing cultures that meet the core needs of staff’ she shared her learning on:
• How we have developed an ‘everyone’ culture – where everyone can belong, thrive and contribute to creating exceptional care.
• How we focus on wellbeing, embedding it into every aspect of working life.
• The impact of this approach and how any health and care organisation can develop positive working environments.
Those who dare – think differently
Everyone culture is about bringing our humanity and care to the work we do together, it’s very simple but it’s not easy – but it’s definitely worth it.
It takes courage, support, dedication and a few good tools.
Belonging – we want everyone to feel safe, to bring their whole selves, to be who they are at work.
We want everyone to be thriving. Meaning we want everybody to be learning, to have a plan, to be able to challenge, to be able to give and receive feedback. To feel they are able to say out loud when something doesn’t feel right. We want everybody to have the opportunity to do work that is really meaningful and purposeful to them.
It sounds simple but it’s challenging, especially whilst operating at this time providing care to people. It takes courage to bring your whole self to work and it takes courage and resilience to learn.
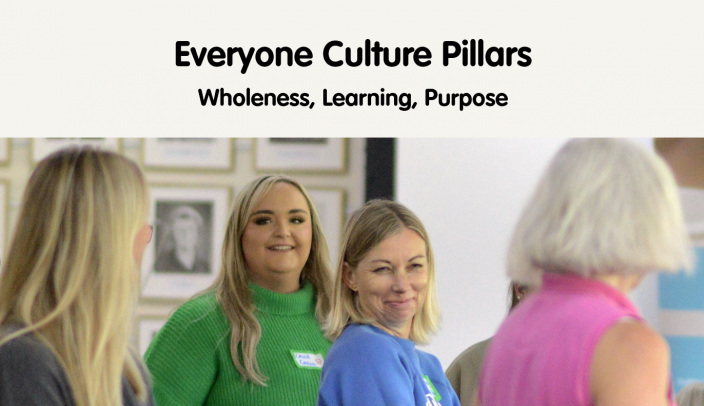
Our pillars
What do we do to support wholeness?
- At the start of each meeting we check in. We bring who we are to the work that we do. People share what’s going on for them – perhaps what’s distracting them. Knowing that we are present for each other means that we can challenge each other better and make more efficient, cleaner decisions.
- Wholeness and wellness work are interlinked. As part of that we have staff led wellness programmes which organises all of our wellness work. For example, we have personal wellness budgets and we provide two lunches a week.
This gives the basis for learning:
- We have learning programmes that are person centred so that everyone has a programme for their own development.
- Our leaders learn in public and they too share their whole selves.
Purpose:
We check in day to day but also throughout the year and ask ourselves really important questions –
Are we doing what really matters? Are we paying attention to what really matters?
One of the ways we do this is by flexible working. As an organisation we place value on what matters to people in the whole of their life – not just whilst they are at work but their lives outside of it as well.
80% work flexible hours in some way
70% work compressed hours
1/2 work part time
And even for those that are full-time there is room for flexibility.
Really putting value in the whole of ourselves and our ability to learn together means we can really serve people with care.
It is challenging – but it is possible.
Too big? Start where you are.
Too difficult? There is no better time to start than now, to be vulnerable and share your feelings. Maybe start with – ‘This feels really hard…’
Vulnerability doesn’t come after trust, it precedes it. Leaping into the unknown, when done alongside others causes the solid ground of trust to materialised beneath our feet. The road to success is paved with mistakes well handled.’ ~ Daniel Coyle, The Culture Code
There is nothing like being held when we make a mistake or being met when you are unsure.
From what we’ve seen in recruitment this way of working speaks to what a lot of people, especially younger people, are looking for: purposeful work and authentic leadership.
Everyone culture is about showing up, telling the truth, asking for help. It’s about using the time you’ve got with a little more courage.
Una Nicholson, Head of People at Here
My role is to support and cultivate a culture where everyone can belong, thrive and do purposeful work where cultures of care extend from our living rooms, to the staff room and the consulting room.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Those who dare: Exceptional care through an ‘everyone’ culture appeared first on Here.
]]>The post Beyond diagnosis – World Alzheimer’s Day appeared first on Here.
]]>Beyond diagnosis – World Alzheimer’s Day

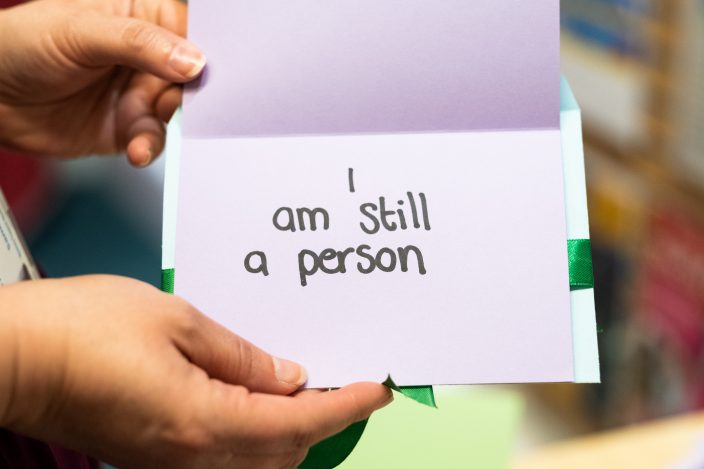
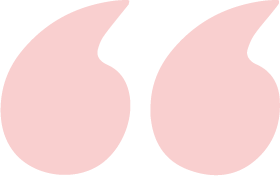
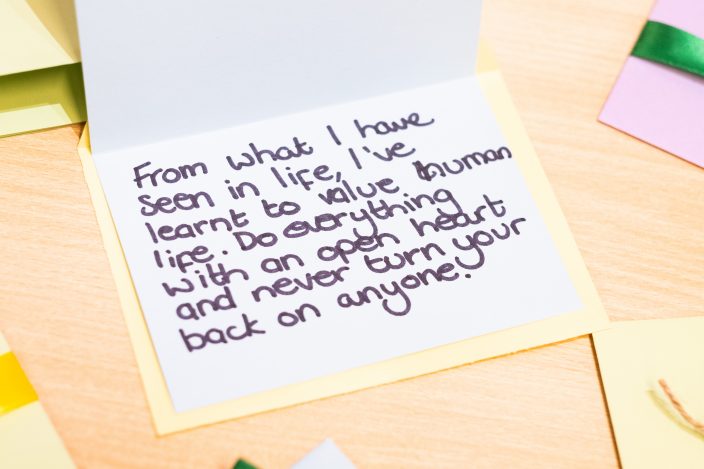
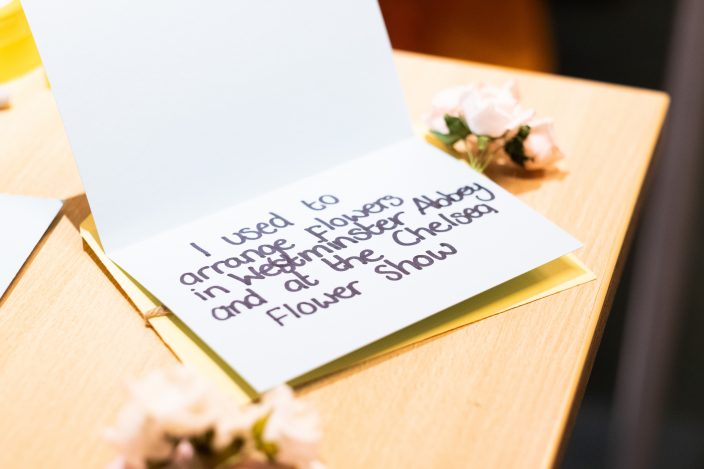
This World Alzheimer’s Day we are encouraged to raise awareness by challenging the stigma around dementia, to look beyond the diagnosis and to see the whole person.
Earlier this year some of the brilliant team from Brighton and Hove Memory Assessment Service (MAS) showcased a poignant art installation at the Jubilee Library in Brighton.
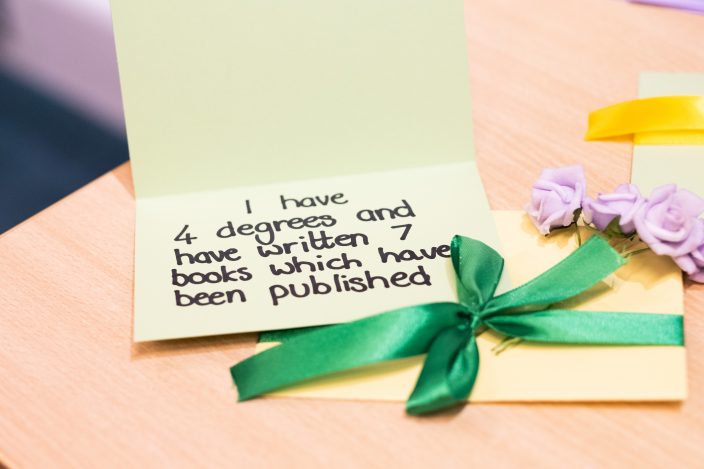
The display was focussed on challenging peoples perceptions of who dementia affects and encourage people to see beyond the diagnosis.
Prior to the event MAS asked their patients the question:

About the Brighton and Hove Memory Assessment Service (MAS)
Brighton and Hove Memory Assessment Service is more than an assessment service, offering both clinical care and social support to those people who are diagnosed with dementia.
It can be a worrying time when you or someone you love begins to experience memory issues. MAS is here to navigate all the ups and downs of adapting to new circumstances, helping people and their loved ones get the care they need to live their life well.
Learn more here.
Get in contact with your GP for a referral.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Beyond diagnosis – World Alzheimer’s Day appeared first on Here.
]]>




