As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
The post Rethinking Our Health: Why it matters appeared first on Here.
]]>Rethinking Our Health: Why it matters

Our CEO explores why rethinking health matters now more than ever and how community-powered approaches can reshape the future of healthcare.
The moment that sparked a quiet revolution
In the summer of 2022, we were deeply inspired by a document from New Local – A Community-Powered NHS co-authored by Adam Lent, Grace Pollard and Jessica Studdert. The principles of community powered health were a clarion call for Here, triggering a quiet revolution in how we delivered our services.
A series of conversations in our clinical teams led to a series of startling innovations across our services, that New Local helped us to take to a wider audience. Our Community Appointment Days approach pioneered in the spring of 2023 is now unquestionably one of our most impactful innovations in delivering healthcare services. More than 120 providers across the UK have now engaged with Community Appointment Days – either adopting the model or actively exploring how to replicate it, changing our expectations of where and how healthcare should be delivered. So, when Adam says what he has written now is the most important thing since then, it’s time for us to take a look.
A healthcare approach based on traditional telling, doing, treating needs a radical rethink
Doing with, not doing to
Doing With: Reinventing Public Services In A Time Of Crisis | The King’s Fund speaks clearly to the challenge of our time – and today we are already in lock step with the approach outlined. Since the earliest days of our services for people with long term conditions we have built in patient leadership. Our staff now known as ‘Health Builders’ are a critical part of our infrastructure – people with lived experience who design and deliver services with the community, enabling the ‘do with’ approach that is so critical to our wider public service reform.
Why healthcare needs a rethink
Nowhere is this more critical than in healthcare. Given 80% of the determinants of health are not related to access to healthcare, a healthcare approach based on traditional telling, doing, treating needs a radical rethink – particularly when it comes to the upstream shift to prevention set out in the ten-year plan. Now, compared to when the NHS was founded, 65% of NHS spending is on long term health conditions.

From treatment to management
What this means is the treatment paradigm needs to shift. For at least 65% of the time, we need to be focused on and enabling ‘management’ over treatment. That means a deep collaboration – led by the citizen, to understand how they want to manage their health condition and integrate this management approach into their daily life, to make sure they have the life that matters to them.
The language of healthcare: time for a rewrite
This frame does not feel shocking to me, and yet the implicit rules that underpin how we deliver healthcare suggest that this approach will be deeply radical. Nowhere is this more present than in the language we use to describe healthcare interactions. We ‘consult, prescribe, treat, review, discharge’. Patients ‘wait, present, comply, disengage or DNA’. We talk in acronyms and euphemisms, about CVD, COPD, CVA, about activation levels, health literacy, risk factors and the ‘hard to reach’.
We treat episodically, with little view of the whole person or their whole lifespan.
Listening with curiosity, humility, and a willingness to let go of assumptions is a radical act, one that can unlock different outcomes.
From patient to person
We ask if they are taking their prescribed medication daily, not if they are walking, talking to others, living in a place they can call home with good work, good friends and a good life.
Only rarely do we connect as humans, acknowledge what matters most, and work together to enable it to happen. Joy, connection, quality of life do not show up in our lists of key performance indicators or our measures of productivity.
Listening is a radical act
Part of what gets in the way is the rigorous training, expertise and experience that sits in the hands of our health professionals. With so much hard-won knowledge and skill, it is challenging to adopt a listening approach, to acknowledge that what we care so passionately about may be of secondary importance to the patient in the room.
Listening with curiosity, humility, and a willingness to let go of assumptions is a radical act, one that can unlock different outcomes.
Charting a new course, Rethinking Our Health project
We know a different approach can work. In the pockets around the country that Adam highlights, new types of conversations are happening, and communities are uniting with new purpose. We’re excited to be exploring how to ‘rethink our health’ in a project at Here. We hope to both design and test new ways of connecting healthcare to communities – to map how healthcare services best ‘dock’ to places and the people they serve is our primary focus.
Alongside this, we want to track how change happens, what makes it possible and sustainable, and to share our learning as widely as we can.
We’re still early in this journey, but we believe this is where the most important work lies, and we’re not alone.
If you’re rethinking health too, we’d love to connect.
We’ll be sharing our learning as the project develops – publishing regular reflections on what works and what doesn’t.
Sign up to updates direct to your inbox
Also of interest
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Rethinking Our Health: Why it matters appeared first on Here.
]]>The post Beyond the Diagnosis: What better care looks like for people with multiple conditions appeared first on Here.
]]>Beyond the Diagnosis: What better care looks like for people with multiple conditions

We know people living with multiple long-term conditions is fast becoming one of the defining challenges of modern healthcare.
Despite the prevalence of complex health needs, care systems are still largely designed around single conditions with separate appointments, professionals, and pathways that rarely speak to each other. For the individual, this can feel like navigating a maze of services with no map.
The King’s Fund’s recent piece on clinical coordination puts this issue into sharp focus. It calls for a shift from fragmented models of care to those built around the person as a whole recognising that people don’t live in silos, and neither should their care.
At Here, we’ve been working to build what this looks like in practice. Whether through integrated musculoskeletal services, faster and more compassionate dementia assessments, or data tools that support local systems to act more holistically, we’ve seen the difference it makes when care is designed for real life, not just clinical pathways.
This blog reflects on the themes raised by The King’s Fund and shares some of what we’ve learned as we try to build care around people, not problems.


1: From care pathways to life pathways
Care that works well for a single condition can quickly become burdensome for a person managing several. Our MSK services in Sussex take a whole-person view—connecting people to physiotherapy, mental health support, community groups, and social prescribing, depending on what matters most to them.
Crucially, this joined-up approach doesn’t just feel better for patients—it’s more efficient for the system. Avoiding duplication, reducing unnecessary referrals, and helping people access the right support first time leads to better outcomes and lower overall costs. Supporting someone to live well with multiple conditions is not just good care—it’s smart use of resources.

Care built around complexity doesn’t have to be more complicated. When we design for real life, we find simpler, more sustainable solutions – for people and for the system.

2. Design with, not for
One of the clearest lessons from our work is that services should be co-designed with the people who use them.
When we partnered with Age UK to deliver a new dementia assessment service, we built it around what people told us they needed: faster answers, fewer handoffs, more clarity and kindness. That feedback shaped everything from the clinical model to the language we use in our leaflets.
The result is a service that feels more personal, more efficient, and more trustworthy.
3. Make the tech work for people, not the other way round
As The King’s Fund rightly notes, good coordination relies on systems that talk to each other—and to the people using them. But all too often, technology ends up serving organisational or system demands rather than patient needs.
We’ve invested in data and analytics platforms that help different parts of the system understand population health and work together. The aim isn’t just efficiency, it’s insight that leads to better, more joined-up decisions.

4. Equity must be built in, not bolted on
People in more deprived areas are more likely to experience multiple long-term conditions—and to face greater barriers in accessing support. Reviewing data with people on the ground tells you where to focus.
By working alongside VCSE collaborators, we’ve created community health days in parts of Sussex where need is high and engagement is low, bringing services directly to people and reducing the friction of navigating formal systems. It’s a small step, but it reflects our belief that access and equity must be considered from the start, not retrofitted later.
5. Relationships matter more than structures
Changing systems is complex. But often, it’s the quality of relationships – between professionals, teams, and organisations – that determines whether care feels joined-up.
In our work, we’ve seen integrated teams flourish when they’re built on trust, mutual understanding, and shared purpose. Creating time and space for professionals to learn from each other and build those connections is just as important as any formal process redesign.

6: Measure what matters – to people and the systems
We’re still too focused on activity and throughput. While these metrics have their place, they don’t capture whether someone feels better, more supported, or more able to manage their health.
At the same time, understanding what matters to people gives us a clearer picture of what works and what doesn’t. That leads to better decision-making, better commissioning, and better value. It means investing in what genuinely helps and scaling back what doesn’t. True efficiency starts with understanding the person, not just the pathway.
Looking ahead
Supporting people with multiple long-term conditions is one of the most complex tasks in modern healthcare but it’s also where some of the greatest gains lie.
When we design care that reflects real life rather than idealised pathways, we unlock better outcomes and better use of resources. Coordinated, whole-person care doesn’t just improve people’s experiences; it reduces duplication, lowers demand on stretched services, and allows professionals to work more effectively.

At Here, we’re learning that care built around complexity doesn’t have to be more complicated. In fact, when we listen to people and work collaboratively across the system, we often find simpler, more sustainable solutions.
We’re excited to be embarking on a new project with The King’s Fund to explore how a deeper understanding of multiple long-term conditions – and more intentional co-creation with the people living with them – can help shape healthcare that works better for both individuals and the system as a whole.
Integrated, person-centred care is not a luxury – it’s essential to delivering quality and value in the NHS of the future.
We’re looking forward to sharing what we learn through our collaboration with The King’s Fund, follow along for open and honest reflections, challenges, and learning as we go.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Beyond the Diagnosis: What better care looks like for people with multiple conditions appeared first on Here.
]]>The post Unlocking better health: The crucial role of personalised care appeared first on Here.
]]>Unlocking better health: The crucial role of personalised care

The importance of personalised care
Personalised Care Week, organised each year by the Personalised Care Institute, is always an opportunity to talk about personalised care – what it is and why it matters.
In many ways, it is extraordinary that in modern health services we need to. After all, what could be more personal than health? What other service needs to be so uniquely tailored to your life?
The decline of individualised healthcare
But over the past century, healthcare has been less individualised – as we focus on better science and better efficiencies, healthcare has become less personal, more remote, and much more transactional than ever before.
In the late 20th century, when New Public Management approaches grew, the NHS, like many organisations, sought to make sure they used their skills, capabilities and resources to the best effect for our populations. So far so good, perhaps.
Except key elements of the market approach fall down in healthcare.
Efficiency and productivity vs. personalised care
In the last few years, conversations about health and care have been resolutely focused on the pressures and demands.
We have been more focused on efficiency and productivity than ever before. And it is impossible to conclude anything other than this is not working.
We are better at pathways, better at flow, have better medicines, more skilled clinicians, better hospital sites. But the health of our nation is failing, and in the words of our own health secretary, the NHS feels broken.
At the heart of this we find an issue illuminated by the language of design – we have fallen in love with solutions, rather than the problem.
Focusing on the root causes of health problems
The problem is not the hip, the knee, the low mood, the high blood sugar, the long wait list.
The problems are personal – they sit more with our lifestyles, our finances, our food and nutrition.
People who are isolated, impoverished, lacking heating, basic amenities, social connections.

With 80% of the determinants of health sitting outside of healthcare services, our focus on better tech, quicker care, slicker pathways may be misguided. In fact, we may be increasing demands – both on services and on the people who receive them.
The role of personalised care in treating multi-morbidities
So Personalised Care Week is a good time to remember this, especially as we focus on multi-morbidities. If you are living with two or more long-term health conditions (like 15% of the population), nothing will be more important than someone taking the time to understand what will improve your health, and how treatment can fit your life.
To deeply understand rather than assume what the problem is, by spending time with those affected. These insights lead to very different definitions of what the challenges are, unlocking solutions that will allow us to tailor healthcare for each and every one of us.
Dr. Helen Curr, Chief Executive at Here
My role is to hold ourselves true to our values. To make sure our commitment to putting people at the heart of their healthcare journey is embedded in every decision and action we take.

Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Unlocking better health: The crucial role of personalised care appeared first on Here.
]]>The post Why do we want to work with hospices? appeared first on Here.
]]>Why do we want to work with hospices?

Hospices have always formed part of my landscape. For a time in Sydenham, St Christopher’s was my next door neighbour, where I grew up in Cornwall, our little back lane now leads to the beautifully designed and uniquely delivered Little Harbour, and I now drive past the stunning new build of St Catherine’s on my way back and forth to my office.
As a healthcare professional, I have long been inspired by the way palliative services resolutely embody the very best of personalised care – with a relentless focus on living, on what is important, on what matters to you and those around you as life comes full circle.
Supporting the hospice sector
Watching the challenges in the hospice sector over the past year has been heartbreaking when you see so clearly the powerful work they do, both to individuals who need their love and care, and to systems who need training, reminders, and inspirational examples of how care can and should be different.
As an organisation Here’s purpose is ‘Exceptional care, for everyone’. We deliver services, but over the years we have also developed offers to support others to deliver exceptional care.
Our focus on data and analytics has long underpinned our innovative services.
Empowered clinicians and patients co-designing services systematically responds to what matters to individuals. Timely accurate data drives every aspect of decision making so care can become bespoke by default, delivering exceptional outcomes and places to work.

Partnering with St Gemma’s Hospice
When we work in partnership we seek likeminded organisations, and it is no surprise that we have started to find these in the hospice sector. We feel privileged to support the work of St Gemma’s Hospice and to share our learning in this new partnership.
In our work with St Gemma’s, we want to bring the full breadth of our experience into the partnership. We will provide a mixture of infrastructure (a cloud-based data warehouse, Power BI), coupled with analytics and other technical expertise.
Our goal is twofold: to streamline St Gemma’s existing reporting processes for greater efficiency, and to harness data-driven insights to better quantify and demonstrate their impact.
By harnessing this data analytics work, we want to help other organisations work more efficiently, empowering them to provide exceptional care not only to the people they support but also to the dedicated staff who deliver care.
Think we could support your organisation? Feel free to get in touch at collab@hereweare.org.uk if you’d like to discuss working in partnership with us.
Dr. Helen Curr, Chief Executive at Here
My role is to hold ourselves true to our values. To make sure our commitment to putting people at the heart of their healthcare journey is embedded in every decision and action we take.

Also of interest
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data rich, information poor: Why analytics matters to hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Why do we want to work with hospices? appeared first on Here.
]]>The post From health inequalities to creating health equity appeared first on Here.
]]>From health inequalities to creating health equity

“By creating a mission around health equity, we can connect our staff to a bolder vision for their work, with healthcare workers as agents of social change, making a difference to our world rather than processing an endless chain of individuals passing through.”
In 1834 Britain passed the Poor Law, an act of Parliament partially creating a safety net for all, but also enshrining a principle of deterring people from making unnecessary demands on public funds that remains present in today’s national debate.
The infirmaries that grew from the poor house would soon be described as “a disgrace to our civilisation” (Lancet 1865) and served as inspiration for the alternative visions of Beveridge and Bevan a generation on.
The Marmot review in 2010 and ten years on (2020), along with the desperately disproportionate impact of COVID show how slow our progress has been.
Poverty continues to kill people in Britain, whether through poor housing (Awaab Ishak: Rochdale housing boss admits 1,800 homes have mould – BBC News), starvation (Disabled man starved to death after DWP stopped his benefits | Disability | The Guardian) or the wider impact of poverty on diet and obesity (Food insecurity as a risk factor for obesity: A review – PMC (nih.gov)) and mental health (Briefing 58: Poverty, economic inequality and mental health – Centre for Mental Health).

Health inequalities today
In today’s Britain, healthy life expectancy remains widely divided between rich and poor with inequities widening since 2010 English indices of deprivation 2019 – GOV.UK
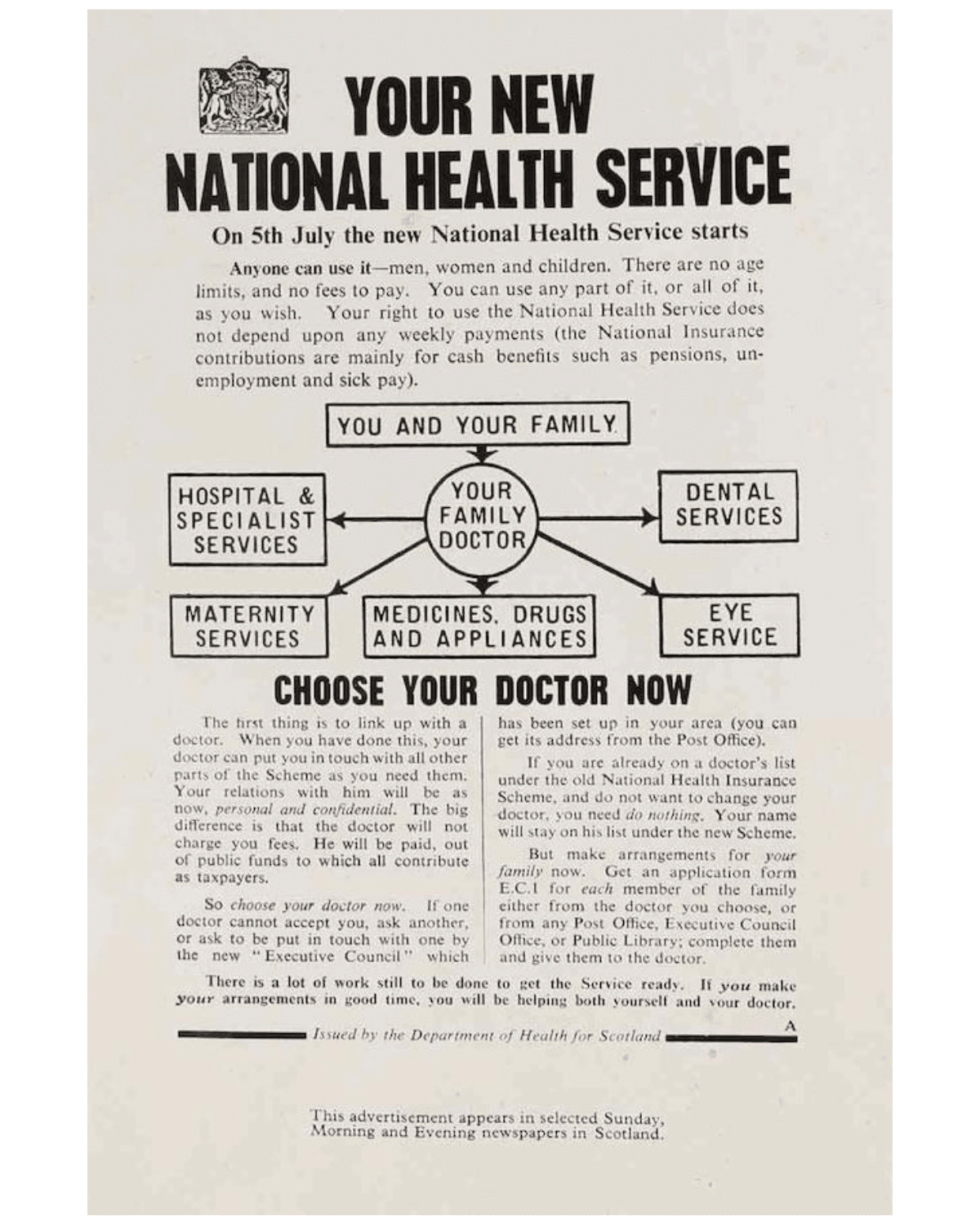
Nye Bevan’s vision for the NHS was a far-reaching reform of access to healthcare, with a more dramatically socialist root than is widely spoken of.
In providing universal access to healthcare, free at the point of delivery, Bevan viewed the NHS as part of an infrastructure that would dismantle division of class and wealth.
When we talk about health inequalities today, we often think of correcting poorer health outcomes, and less about social justice.
There is a risk that we fail to recognise in real terms the need to deliver more (and different) health and social care interventions for some people, rather than just making sure there is equal access to the traditional offer.
Shifting the language from health inequalities to creating health equity
More insidiously, at times of high demand, services can pivot to the quick wins, trying to reduce overall waits or meet blunt targets. At these times, delivering care to groups with different needs can feel more challenging, ‘complex’, and bypassed on route to the ‘low hanging fruit’.
During the rollout of the COVID-19 vaccine, we saw this in real time, with data tracking how some populations accessed vaccine quicker than others, and the cost of delivering to some groups was higher – and therefore not incentivised in a fixed tariff payment mechanism.

Wider than this, we know the presence of health conditions or caring responsibilities adds disadvantage over time, a vicious cycle where 54% of carers report their own health had suffered, and 44% had put off seeking health treatment because of their responsibilities. For these groups ‘equal’ access to treatment as usual will not meet their need.
Shifting the language from health inequalities to creating health equity paints a much broader picture.
It engages our services in recognising that part of the mission of the NHS is a social justice one, that we are a part of how wealth is re-distributed, by providing safe, universal, free access to healthcare, we can balance the accident of birth. As Marmot says, “if health has stopped improving, it is a sign that society has stopped improving”.
Healthcare workers agents of social change
By creating a mission around health equity, we can connect our staff to a bolder vision for their work, with healthcare workers as agents of social change, making a difference to our world rather than processing an endless chain of individuals passing through.
From this lens, we are stretched to consider what more we can do, taking proactive approaches to the delivery of health, seeking out places and populations who we know are disadvantaged, and playing our part in levelling the playing field.
With this focus, our task is shaped differently. No longer do we look at access data in terms of whether it is representative of our population, but whether it is representative of our population need.

Our programs and services spend more in areas of deprivation, understand that delivery methods than may be more expensive, and focus on the value this represents in lifting the disproportionate distribution of wealth (in its widest sense).
Doing things differently for a better world
More contentiously it could mean sifting through these long waiting lists differently – to identify those who are disproportionately impacted, less advantaged, less resilient, less able to wait, in service of a fairer society.
It is as much part of our social mission as it is our commissioned services, and we want to do more. We are not alone. Despite all of the pressures within the NHS, we know there is a growing emphasis and commitment to the pursuit of a better world, a drive for health equity at every stage of our lives.
Through our data dashboards and outreach programs (Vax and CAD), we have learned about how to deliver healthcare differently. Delivering quick, efficient healthcare to the many, and bespoke, targeted offers to the few.

We believe we’re stronger together. If you’d like to work with us to find new and innovative ways of growing health equity then we would love to hear from you.
Get in touch: collab@hereweare.org.uk
Dr. Helen Curr, Chief Executive at Here
My role is to hold ourselves true to our values. To make sure our commitment to putting people at the heart of their healthcare journey is embedded in every decision and action we take.

Also of interest
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Our Health: Why it matters
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.
Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.
The post From health inequalities to creating health equity appeared first on Here.
]]>The post What if we made community powered health, for everyone appeared first on Here.
]]>What if we made community powered health, for everyone

As a social enterprise our purpose is to create exceptional care, for everyone.
We are incredibly proud of the services we deliver, and sharing our learning is an important part of our culture.
Many businesses talk about growth, for us, we measure that in terms of impact, as well as delivery.
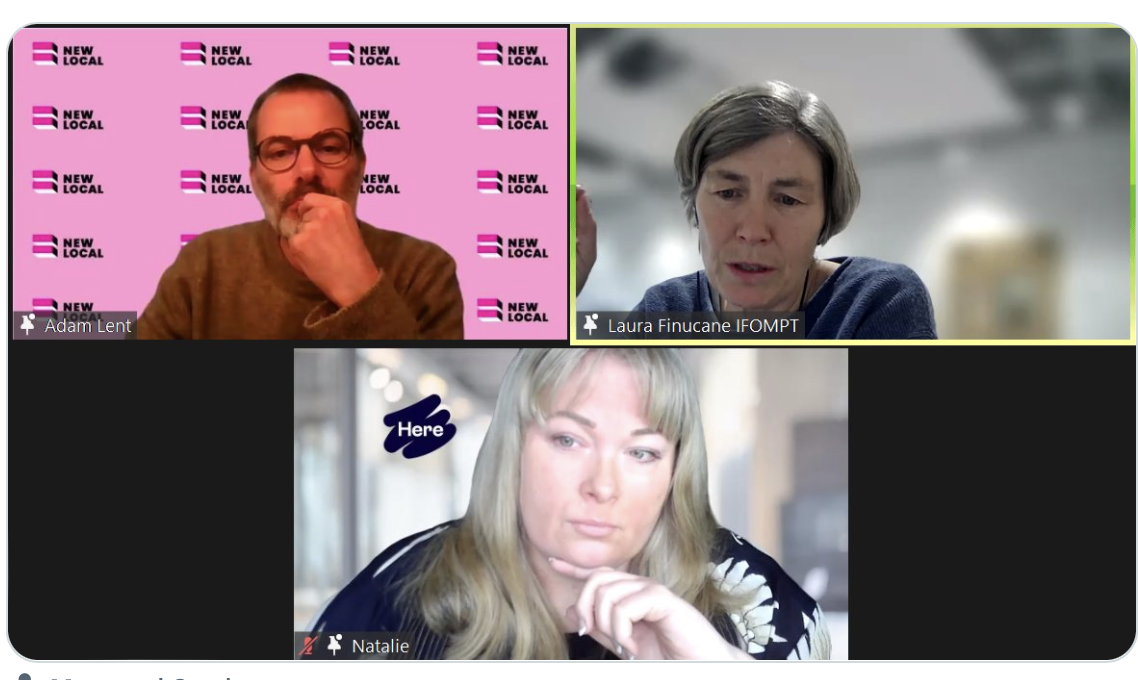
That’s why we were so excited about our New Local webinar this morning, talking about our Community Appointment Day innovations in Sussex.
Today over 270 people were on the call, with the wonderful Natalie Blunt and Laura Finucane talking about how they got the CAD up and running, and what impact it had.
Whilst we are still tracking our data, and learning what works, what I’m left with this morning is the incredible news that across the country, CADs are popping up like mushrooms.
What started as a ‘what if’ conversation in our teams, is becoming an accepted idea – fuelled by a desire to experiment, to try something different, knowing that doing what we’ve always done will not solve the problems we face.

Its not just in MSK, and its not about waiting lists. Creating new ways to deliver truly personalised care is an idea our systems are ready for. Common sense innovation, that anyone can read about and think – how might we do that around here?
As a social enterprise, this is what we are about. Business for good. We’re excited to connect with others who are exploring this idea. We’re happy to share, and importantly we’ll learn from how this idea develops in other places.
Creating exceptional care for everyone is going to take change on a new scale. Strength based, community powered health.
Whether you’re daunted, deliberating or determined to try, we’d love to be connected.

Want to learn more about the Community Appointment Day model?
For more information please contact us: collab@hereweare.org.uk
Read about how it all started in our blog: Community Appointment Days – An idea that rapidly turned into an innovation
Dr Helen Curr, Chief Executive
My role is to hold ourselves true to our values. To make sure our commitment to putting people at the heart of their healthcare journey is embedded in every decision and action we take.

Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post What if we made community powered health, for everyone appeared first on Here.
]]>Creating long term health: Four key ingredients for a different approach

Medical approaches to health commonly diverge around acute and chronic presentations. What I need after an unexpected accident, a short illness or a new concern is very different from when I am living with a condition long term.
In an acute illness, rapid, transactional models of care are effective – even welcome – lives are at stake, care is short term, and expertise largely sits with the trained professional.
Translating this mode into chronic care is filled with risk. A chronic condition affects our whole lives, from morning to night, throughout the seasons. Any treatment approach cannot be simply prescribed from professional to patient, and compliance monitored. We need to flip the lens – any treatment regime needs to ‘comply’ with our lives – what is important to us and what can be sustainably incorporated into our unique set of circumstances.
The perfect treatment approach for one, can be radically flawed for another. Humans do not come in neatly packed boxes.

This challenge of what makes the right health collaboration is what makes us tick at Here. We are inspired and driven by the right combination of skills that builds health – the collaboration between experts–by–experience and health professionals, that has peak potential in working with long term conditions.
Now more than ever before, this is where we focus our time. So what sits at the heart of this approach?
It breaks into 4 key pillars:
1: What Matters To You
This is at the heart. Conversations, not consultations. Every contact with every patient is started focused on knowing what matters most – an honest and safe space to match their personal experience, hopes, aspirations and obstacles, with the knowledge and skills a professional might provide. It sounds simple, and it many ways it is. It takes a commitment to putting your needs as a clinician, an administrator, a busy health professional second place, making sure value to the patient is the offer on the table.
2: True collaboration
Every individual conversation is a collaboration. Shared decisions with people seeking care are made and ways forward devised. Then we learn, we change, the service and our partnerships evolve. The people who use our services become part of our infrastructure – with paid roles bringing deep expertise.
This isn’t ‘representation’, we invest time and resource in people who have the skills we need – we co-design, improving the services we provide because we have access to a secret weapon – the inside track of what it is like to receive them. We do this, not just because it is the right thing to do, but because it is the smart thing – our services are better – for the people who use them, the people working in them, and the communities they serve.

3: Our data
We believed our approach would be better. Now, we know that it is with real time data, available to all, that tracks outcomes. It tells us what works, and what our populations need. It lets us manage our resources well, particularly in services under pressure. Our data enable us to create equity by design. All our services generate and report data on who uses them, and who doesn’t, driving us to take action to reach the people who may need us most, and who are least often served well. Smart data system drives real change in the world.
4: Our approach is sustainable
A temporary pilot, that leaves no lasting legacy of change waste opportunity, effort and resource. Our world is changing, and that’s why we have a continuous approach to innovation and improvement. We have to take the best of the innovations and bake them in to our service design. Complex repetitive tasks are prone to human error, we use the best technology to free precious time for clinicians and care staff to invest in human and unhurried connections.
We are committed to connecting to people all over the world who are innovators in health. We learn wherever we can, and where evidence is not available, we set out to experiment and find solutions ourselves.
We share what we find, taking pride when others adopt approaches we have road–tested. Working with partners, we can step in, and out of delivery. We work alongside anchor institutions and community groups who may be taking this work forward long after our role is complete.
If it sounds right, intuitive, that might be because it speaks to what you would want to build a healthy life. Driving these principles through what we do every day, is what keeps us here, working in health, every day.
It inspires us to better things, and it’s the beating heart of exceptional care, for everyone.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Creating long term health: Four key ingredients for a different approach appeared first on Here.
]]>The post Community Appointment Days: What makes them tick? appeared first on Here.
]]>Community Appointment Days: What makes them tick?

Common sense innovation is one of our by-words at Here – we believe in innovation, and doing things differently – we also believe in simple ideas that have great impact.
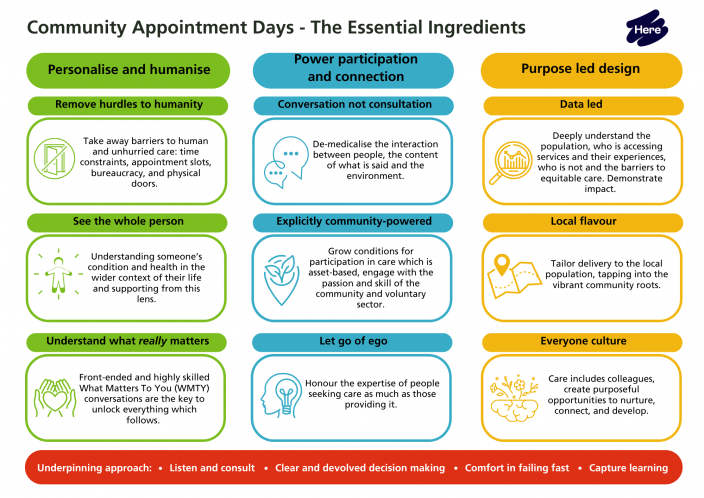
Community Appointment Days (CADs) are a simple idea, built on a bedrock of partnership, personalised care and devolved decision making. With all eyes on the growing NHS waiting lists, anything that serves to get people quickly to the care they need is gathering attention.
But what makes them work? Could this happen anywhere?
These are my reflections on the story so far:
Partnership is key
As a social enterprise, we’ve been working hand in hand with our Sussex Community Foundation Trust (SCFT) colleagues for over ten years. At the CAD you can tell. Everyone introduces themselves as MSK Partnership staff. One team, not several. Everyone pulling together.
We draw on the agility and creativity of a small social enterprise and join forces with the expertise and credibility of the NHS. A perfect example of the whole becoming more than the sum of its parts.

MSK practitioners at a Community Appointment Day (CAD)
Personalisation is the difference
As an organisation our calling card is exceptional care for everyone. We specialise in personalised care approaches to long term conditions. We constantly ask the question – is this care exceptional – both in terms of the standard of care, and our ability to make an exception to respond to a particular set of needs.
The MSK partnership has a mission too – putting patients at the centre of their healthcare journey. Why does this help? It means we focus only on understanding what really matters to someone, and this has been the beating heart of the CAD.
Making sure we understand, and quickly respond to the things that are going to make a difference, and not wasting any time offering or pursuing pathways that just don’t suit.
I liked the atmosphere and behaviour of staff. Everyone was lovely and anxious to help me. I liked both areas I was sent to, especially rehab because the lady there was extremely kind and went above and beyond with trying to help me.

Devolved decision making
If you are going to really be person-centred, and allow for shared decision making with people, your clinical team will need the autonomy and independence to enact creative thinking every day. By baking in clear vision and values in every part of the system, you can trust teams to do what matters.
As a clinician you know that so long as you are holding true to the values, you have a great deal you can offer. Good for managers, good to staff, good for people.
Simple rules let you work with complex problems – and when it comes to caring for people, each and everyone of us arrives with our own complexities to understand.
I found each area really helpful, every member of staff I saw was sympathetic, understanding and amazing. I felt listened to and not judged.
A learning culture
You know the saying, ‘Culture eats strategy for breakfast?’ If we’d set out two years ago with a strategic plan to reduce our wait list, it’s unlikely we’d have come up with this. If we’d had board sign off from all our partners, this idea would still be sitting on a table waiting for final governance sign off or a pilot.
By creating a culture of working in teams to solve day to day problems together, guided by principle but supported by robust data and learning, we have teams who are unusually used to trying out new things. This ability to quickly learn, try and fail, change tack means we are improving all the time.
The CAD days evolved from a clinical validation approach that wasn’t working well. Our approach to learning meant we identified the piece that was working – the what matters to you conversation – sowed the seed for a whole day focused around this one conversation.
Find out what people had to say after attending a Community Appointment Day here.
Download the Community Appointment Day Essential Ingredients.
About Sussex MSK Partnership Central
Sussex MSK Partnership Central is a joint venture between Here, & Sussex Community NHS Foundation Trust. This is a prime contracting model supporting musculoskeletal (MSK) health for a population of 650,000 covering physiotherapy, orthopaedics, rheumatology and chronic pain. The service operates across central Sussex; including Brighton & Hove, Horsham and mid Sussex and Crawley.
Website: www.sussexmskpartnershipcentral.co.uk
Interested in finding out more about the Community Appointment Days?
Email collab@hereweare.org.uk or use the form below.
Get in touch
Interested in learning more about our services, programmes and innovations? Fill out the form and we’ll get in touch.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Community Appointment Days: What makes them tick? appeared first on Here.
]]>






