As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
The post Early Pain Support: Insights From our first Community Drop-In appeared first on Here.
]]>Early Pain Support: Insights From our first Community Drop-In

As part of Rethinking Our Health, we hosted our first community pain drop-in, a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. Laura Finucane shares what we learned, and why having the right conversation at the right time really matters.
As part of Rethinking Our Health, we recently hosted our first pain drop-in session. It was a simple idea, but one rooted in a powerful principle: if we support people early, with the right advice and reassurance, we can help them feel confident to manage symptoms before they escalate into something more complex.
The drop-in is designed for people experiencing acute or early pain that has been present for less than 12 weeks. It offers an informal, preventative conversation rather than a clinical appointment. This is not a clinical service, nor a replacement for existing care pathways. Instead, it operates upstream of formal services, supporting people before they feel the need to seek clinical intervention.
By providing trusted, evidence-based advice, guidance, and signposting at an early stage, the drop-in helps people build the confidence and capability to manage symptoms themselves. Traditionally, early pain support sits within primary care, where timely access can be challenging. This approach creates space earlier in the pathway, reducing reliance on clinical services by ensuring people have the right tools at the right time.
Strength-based conversations
conversations were grounded in a strength-based approach, focussing on understanding what was important to each person and working together to agree next steps. Rather than telling people what to do, we supported them to make a plan that made sense in their own lives.
That sense of partnership is critical. It builds capability, not reliance, and reinforces the message that people are not passive recipients of care, but active participants in their own health.
Building confidence, not dependence
Most wanted reassurance, clarity, or guidance on what to do next. They wanted to sense-check their symptoms and understand whether what they were experiencing was “normal,” and how best to respond.
Several people told us that had the drop-in not been available, they would have booked an appointment with their GP. After talking things through, they no longer felt they needed to. They left with practical tools, clearer understanding, and the confidence to manage things themselves. That is exactly the upstream impact we were hoping for.
This is about prevention in its truest sense: supporting people early so they do not need to access services later because they already have what they need.
Challenging outdated beliefs
One of the most striking themes was how persistent some outdated messages about pain still are. Bed rest, for example, has not been recommended for acute back pain since the 1990s, yet we repeatedly heard that people believed resting completely was the “right thing” to do – and many were actively doing it.
These conversations highlighted how valuable early, trusted advice can be. Simply correcting misconceptions and explaining why movement, pacing, and reassurance matter can make a significant difference to how someone experiences pain and recovers from it.
Seeing the whole person
Pain rarely exists in isolation, and the drop-in reflected that. Access to social prescribers and community workers meant that support went beyond musculoskeletal pain alone. Around a third of people attending were signposted to wider community support, recognising the social, emotional, and practical factors that influence pain and recovery.
This broader approach makes a difference. When people feel supported in the things that matter to them – their work, caring roles, mental wellbeing, or social connection – they are better equipped to manage physical symptoms too.
A small intervention with big potential
This first drop-in reinforced why rethinking how and when we support people matters. By going upstream, by normalising early conversations, and by sharing trusted, evidence-based advice in a community setting, we can build confidence, reduce unnecessary demand on services, and help people feel more in control of their health.
For me, this is what Rethinking Our Health looks like in practice: meeting people earlier, listening carefully, and ensuring they leave feeling reassured, informed, and supported.
If you’d like more information about The Community Pain Drop-in, or Rethinking Our Heath
drop us a line at collab@hereweare.org.uk
Also of interest
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Early Pain Support: Insights From our first Community Drop-In appeared first on Here.
]]>The post New RCGP Report Highlights Hidden GP Workload appeared first on Here.
]]>New RCGP Report Highlights Hidden GP Workload

The Royal College of General Practitioners (RCGP) has published a compelling new study, “Uncovering the GP workload burden: A study of the drivers and costs of unnecessary and hidden workload” (December 2025) and we are proud that Here is featured as a key research partner in this landmark work.
Commissioned by the RCGP as part of its strategic priority to better understand and address workload pressures in general practice, this report investigates the nature, scale, and impact of what it terms “unnecessary” and hidden workload, work that absorbs valuable GP time but adds little direct clinical value.
Key Findings of the RCGP Report
The RCGP study deploys a thorough mixed-method design, including literature review, interviews with practitioners, and time-and-motion analysis, to produce insights into what kinds of tasks are consuming GP time and how these affect capacity and morale.
Among the most striking findings:
- Hidden workload is significant. Tasks characterised as unnecessary or inefficient, such as form-filling, navigating fragmented referral systems, and external administrative requests, were pervasive and often time intensive.
- Costs are material. Using time-and-motion data, the study estimates the average daily cost per GP attributable to unnecessary activities, at £410.53, a measure that underscores the operational and economic impact of the issue.
- Impact on Wellbeing and Retention. Beyond time and cost, the report highlights that unnecessary workload contributes to emotional fatigue, burnout risk, and reduced job satisfaction; factors that are central to contemporary concerns about GP recruitment and retention.
Why this matters, and what Here is doing about it.
While the report does not claim that all administrative or non-clinical tasks are avoidable, it does illuminate the complex interplay between system design, external demands on GPs, and the realities of practice workflows.
For Here, this research affirms our conviction that better data, rigorous analysis, and practical insight are essential to designing interventions that truly reduce unnecessary burden without compromising quality of care.
Our involvement in this RCGP research has both informed and strengthened our internal product and analytics strategy and we continue to:
- Partner with healthcare organisations and frontline practitioners to refine workload measurement frameworks.
- Embed research findings into the development of solutions that support workload-intelligent operations.
- Advocate for evidence-based policy that recognises both the value and the cost of hidden clinical work.
Here’s Role in the Research
Working collaboratively with researchers from Apollo Innovation, Here was commissioned to contribute analytical expertise and co-design elements of the mixed-method research approach underpinning the study.
Acknowledgements
We thank the RCGP and all participating general practices for their collaboration on this important study. We also congratulate our colleague Ann Ahmad for her expert contribution to the report, which reflects Here’s commitment to evidence-led impact in healthcare analytics.
To find out more or to chat with our analytics and products team, drop us a line
Also of interest
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data rich, information poor: Why analytics matters to hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post New RCGP Report Highlights Hidden GP Workload appeared first on Here.
]]>The post Data and Analytics: why we work with hospices appeared first on Here.
]]>Data and Analytics: why we work with hospices

Exceptional care, for everyone
At Here we talk about our purpose being ‘Exceptional care, for everyone’. As well as providing outstanding clinical services, we deliver on that purpose through partnering with other organisations to deliver the ‘outstanding’.
This has always been part of our ethos. Most of the work that we do is in partnership with others, and it’s a way of working that feels engrained in what we do.
Connecting with hospices
The connection with hospices grew out of various enquiries that we had received about working with TPP SystmOne data. Many hospices had transitioned to the SystmOne Electronic Patients Records (EPR) in the last 5 years, and there seemed to be a common question – “we have lots of great data, but how do we use it?”
That resonated with us: SystmOne is a very ‘grown up’ clinical system – it is highly customisable, and the volume and sophistication of the data is captures is impressive, so much so that getting the best out of the data can be complicated.
That was our story as well – we have been using SystmOne successfully for around 12 years, and we realised very quickly that we needed to make investments in our analytics skills and infrastructure to make it work in the way that we wanted.

What are the analytics needs of hospices?
The message comes through loud and clear: hospices don’t want someone to do data analysis for them—they want to do it with them.
This distinction matters enormously. Hospices are working within tight resource constraints, but they’re hungry to build their own capabilities. The journey they’re facing is familiar to many healthcare organisations: moving from spreadsheets to Power BI, and scaling to data warehouses. It’s not just about the technology though—it’s about upskilling teams and building confidence in working with data.
Accelerating digital strategy
We’ve learnt that what hospices are really seeking is an accelerator, not an outsourced solution. They want to learn from someone who’s navigated this path before, avoiding the pitfalls and focusing on what actually works in a healthcare setting. There’s a recognition that sustainable change comes from building internal capability, not dependency on external consultants.
Right now, digital and data strategy isn’t just nice to have—it’s absolutely critical. Hospices are increasingly viewing data as a strategic asset, not merely an administrative burden. With healthcare systems under unprecedented pressure, hospices need to demonstrate their value and impact through evidence.
This is about more than efficiency or reporting. It’s about enhancing the visibility of hospice care within the broader health system. When hospices can clearly articulate their outcomes, resource needs, and the gaps they’re filling, they strengthen their position as essential partners in end-of-life care.
The challenge ahead is clear: building data capability within resource constraints, but the appetite for change has never been stronger.
The challenge ahead is clear: building data capability within resource constraints, but the appetite for change has never been stronger.
What did we learn?
The pressure is mounting. NHS standards and mandatory data returns are creating new demands on hospices that can’t be ignored. While every hospice we’ve worked with shares fundamentally similar needs, they’re each at different points in their data journey.
A cookie-cutter approach simply doesn’t work. Each hospice has configured their systems differently, grown organically with different tools, and faces unique local constraints. What is transferrable isn’t a plug-and-play solution—it’s the underlying knowledge. Understanding how to connect disparate systems behind the scenes, how to make data flow smoothly between platforms, and how to overcome the messy, real-world challenges that data inevitably throws up.
We’re seeing some promising collaboration emerging at regional level, though it’s still in early stages. Hospices are beginning to recognise the value in sharing approaches and learning from each other’s experiences.
The priorities are becoming clear across the sector. Hospices are focusing on population health management, improving access and equity for their communities, understanding IPOS (Integrated Palliative care Outcome Scale) effectively, and developing robust impact measurement. These aren’t just buzzwords—they’re the foundations for demonstrating value and securing the future of hospice care.
Get in touch for an informal chat about how we can help you transform your analytics:
Analytics@HereWeAre.org.uk
Also of interest
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data rich, information poor: Why analytics matters to hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Data and Analytics: why we work with hospices appeared first on Here.
]]>The post Rethinking Our Health: starting with pain appeared first on Here.
]]>Rethinking Our Health: starting with pain
Our latest update from Jo Crease, Programme Manager at Here, shares our progress on Rethinking Our Health, a community-led approach to improving support for people living with long term conditions.
Picking up from the co-design sessions at the start of summer, Jo explains where we’ve got to since then, what we’ve learned from communities about MSK pain, and what we’re going to test next.
Rethinking Our Health – so, what are we actually going to do?
Over the summer, people have quite reasonably been asking what Rethinking Our Health is actually going to look like in practice. What are we going to do, where, and with who?
I’ve spent much of the last six months saying: “We don’t know yet, because we haven’t asked the community yet – and that’s the whole point!”
Now we’re at a point where we have asked the community, and this is what happened next.
A reminder: what is Rethinking Our Health?
Rethinking Our Health is our shared programme with The King’s Fund to explore new ways of supporting people with long term conditions, starting from what communities say matters most.
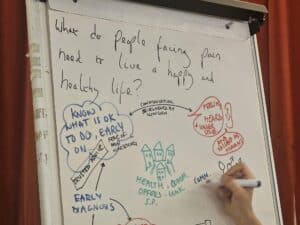
How we’ve been working with communities and VCSE partners
Over the past few months, we’ve been in rooms with community members, VCSE organisations and partners, testing ideas together and challenging our own assumptions – rather than deciding solutions from the centre. After these sessions, all the collaborators came together to make sense of what we’d heard, compare insights and pull the learning into one shared picture.
Why we chose to start with pain
We all agreed we wanted to improve support for people with long term conditions – and we chose to start with “pain” as a way to talk with and support people who were struggling to get what they need.
But the priorities weren’t always the same.
Here and The King’s Fund were thinking about the longer-term challenges in how health and care needs to work in future. Our test site partners were focused on the immediate reality of people not being able to get what they need right now.
Once we recognised that difference, the question became: how do we create something that works for both?
We tried to square that circle by starting from the community’s point of view and seeing how that could lead towards more sustainable solutions for the NHS.

What we learnt from truly listening to communities
As we tested ideas locally, a pattern emerged.
In spite of our best intentions, we were still coming across as “here’s something we’ve designed for you”, rather than “here’s how we want to build with you, starting from where you are right now”.
There was also a clear expectation that anything we offer had to genuinely solve problems people already face and not feel like yet another ask for people with busy lives and services that are already stretched.
We also learnt that creating new roles, like ‘Champions’, wouldn’t be welcome. People are already active in their communities, with their own motivations and networks. They don’t necessarily want another label or obligation – especially one created by public services rather than driven by what actually matters locally.
Community development organisations work because they start with what people already have: their strengths, motivations and contributions. They don’t impose new ones.
This feedback was honest and challenging, but it came from trust. We’ve worked hard to build that trust over the last six months, and because of that, partners were able to give this critique, and we were able to hear it – and act on it. And we know the work is stronger because of it.
Our response: a three-part community offer on early pain
People told us they wanted:
- Trusted advice, early enough, local and accessible
- A way to understand more about MSK pain
- People working in the community being part of a solution together
Working with our test sites, we’ve refined the goal to build neighbourhood-level awareness, capacity and confidence to act on early pain. And we’re doing this through three interlinked elements that are, crucially, built on existing community assets and relationships.
1) Trusted advice, early enough, local and accessible
Community Health Drop-In
A weekly half-day drop-in hosted by a Community Development Worker, with a physio and a social prescriber. This is a space for advice, guidance, support with social factors and community connection.
2) A way to understand more about MSK pain
Community learning and peer support
Four modules covering: pain management, medication, exercise and movement, and general health and wellbeing. We are using a train-the-trainer model so community workers can deliver these sessions in the longer term.
3) People working in the community being part of a solution together
Workforce learning offer
A CPD-accredited short training offer for people working in the community – primary care, VCSE, social care, libraries, food banks and volunteers – building confidence around early pain and health coaching and encouraging neighbourhood networks around pain.
What happens next
It’s still very much a work in progress – we need better names for the elements of the offer for a start (drop a comment with suggestions!).
We’re going live mid-November and running through to March in the first instance. The next update will share reflections from the first Community Health Drop-In. I’ll also be talking about how we plan to balance getting the data we need without overloading participants, and how we’ll involve community researchers in understanding people’s experiences of this work more deeply.
As always, let us know what you think – what questions do you have?
Drop us a line at collab@hereweare.org.uk
Want to follow the journey?
Sign up to updates direct to your inbox
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Rethinking Our Health: starting with pain appeared first on Here.
]]>The post Rethinking Pain: Insights from The Kings Fund and Here appeared first on Here.
]]>Rethinking Pain: Insights from The Kings Fund and Here

Pain is too often treated as a symptom to suppress. But what if pain itself were a signal – an opportunity to intervene early, support people now, and prevent more complex health problems later?

A “Do With” approach
The blog argues for a fundamental shift: from doing things to people in pain, to doing things with them. That means co-designing services alongside people with lived experience, understanding what really matters to them, and supporting them to take part in shaping their care. This approach resonates deeply with our work at Here, where we are rethinking how pain services can be delivered across Sussex and beyond. We know that pain doesn’t exist in isolation — it affects movement, sleep, relationships, mental health, and overall wellbeing. Addressing it effectively means working across boundaries and building partnerships that help people stay active, connected, and in control of their health.
Shaping pain services for the future
Our Rethinking Our Health programme is already putting these principles into practice:
- Co-production: involving people with lived experience of pain in designing, testing, and improving services.
- Holistic support: integrating physical rehabilitation with psychological and social support.
- Prevention focus: identifying and responding early to help reduce the long-term impact of persistent pain.
- Accessibility: ensuring that services are easy to reach, responsive, and equitable.
This collaboration with The King’s Fund reflects our shared belief that meaningful change happens when people, professionals, and communities design health services together. You can read the full blog, “Rethinking Pain: Can a ‘Do With’ Approach Prevent Complex Multiple Conditions?”, on The King’s Fund website.
If you’d like explore how we’re
rethinking pain services
drop us a line at collab@hereweare.org.uk
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Rethinking Pain: Insights from The Kings Fund and Here appeared first on Here.
]]>The post Experiencing Exceptional Care in Sussex: A Mother’s Story appeared first on Here.
]]>Experiencing Exceptional Care in Sussex: A Mother’s Story

Lesley’s experience with Sussex Community Dermatology
At Here, we believe that exceptional care starts with understanding ‘what matters to you’. When people feel seen, heard, and supported to express what’s important, they become active partners in their own care, and that’s when real change happens.
Lesley Jay, our Finance Director, recently experienced this first-hand when she took her 14-year-old daughter to the Sussex Community Dermatology Service, run from Bersted Green Surgery in Bognor. Here she tells us how this felt for her and daughter and the difference it made for them.
A warm welcome that set the tone
“I recently had such a great patient experience when I took my 14-year-old daughter for her first dermatology at the Sussex Community Dermatology Service, that I had to share it.
From the moment we walked into the GP practice, we were met with warmth and kindness. The receptionist looked up, smiled, and said, “You must be Isabella!” directly to my daughter. Her face lit up as she was the focus, not me. The receptionist told her that they were running about 20 minutes behind because some patients had needed extra time and asked if that was okay with her.
It was such a small thing, but it made a big difference, subtly telling my daughter that her time and her needs mattered, and that if she needed extra time too, that would be okay. She sat waiting for her appointment feeling calm and cared for, before it had even begun.”
He talked with her, not about her
An empowering conversation
“When we met the consultant, Dr Jonathan Sutton, he began by asking about her life outside of school — what she enjoyed, what she liked to do. That small conversation put her at ease and opened the door for her to talk honestly about her skin, how it affected her confidence, and what had or hadn’t worked before.
He talked with her , not about her to me. He really listened to what she wanted from her treatment and supported her to make the choice that felt right. She left with a prescription she was confident in, and, more importantly, feeling in control of her treatment.”
Building on what matters
“For a shy teenager, being put at ease, treated with respect, and invited to speak up was transformative. That first encounter built a foundation of trust and optimism that will support the success of her treatment going forward.
Now our follow-ups use local blood tests, simple digital surveys, and virtual appointments, building on that shared understanding of what matters to her.
For a shy teenager, being put at ease, treated with respect, and invited to speak up was transformative.
Why understanding what matters – matters
Stories like this remind us that the best healthcare experiences don’t just treat a condition -they start with understanding what matters to you.
That’s the principle at the heart of everything we do at Here and it we love to celebrate exception care when we come across it. We believe it’s important to identify, celebrate and learn from exceptional moment of care like this one.
Because when we start with what matters to you, everything else follows.
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Experiencing Exceptional Care in Sussex: A Mother’s Story appeared first on Here.
]]>The post Data rich, information poor: Why analytics matters to hospices appeared first on Here.
]]>Data rich, information poor: Why analytics matters to hospices

Changing landscape
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data & analytics as if they are.
Faster Data Flows
For example, programmes such as ‘Faster Data Flows’ designed to provide and share timely data across care providers, Integrated Care Boards (ICB’s) and NHS England to ‘improve the flow and speed of data to support local, system and national decision making’. Quite rightly, hospices are being asked to participate, and it is important that they do, because that’s what it means to be part of the NHS data landscape, and the NHS pays for what it can see.
But this places a burden on hospices to either take on more manual processes and administrative burden, or do the necessary system configuration and data engineering in order to connect in this way. A typical hospice may have one or two analysts, but is unlikely to have the data engineering expertise to hand

Analysis Paralysis
The good news is that most hospices have now migrated to modern Electronic Patient Record (EPR) systems. These systems are typically the same as those used within NHS primary and community care, so data is likely to be collected in the same way. In fact, when configured correctly, these systems have potential to hold vast amounts of information concerning every aspect of patient care.
The tricky part is that it isn’t that easy to get the data out and use it. Using tools like Excel (or even Power BI) is quite rate limiting unless the data has been properly structured outside the EPR. Put simply, the analyst resource available will be used up just trying to maintain relatively small numbers of reports – checking anomalies, trying to cope with changes to the data that break everything – when it should be purely focused on what adds most value – measuring impact, helping people to do their jobs.
Well, the other good news is that it isn’t that hard to break out of Analysis Paralysis.
Opportunity
So what is the solution? What does exceptional analytics look like? Is it affordable when hospice finances are stretched to, and in some cases beyond, breaking point?
Having invested resources to migrate to modern EPR solutions, analytics is really the icing on the cake and much more achievable than it might appear. The things that get us there are:
- Using a data warehouse to load and ‘transform’ the EPR data in a way that makes it easier for analysts to use and provides a ‘single version of the truth’ – fix the data in one place, rather than in every report and spreadsheet that it gets used in
- Link in external datasets such as population demographics to better understand how they meet the needs of their community
- Make the data securely available throughout the organisation through a business intelligence platform like Power BI, Qlik Sense, or Tableau to provide information to anyone that has a need – managers, clinicians, directors – with bespoke dashboards and reports that can flex and evolve through time. If the analysts are spending 80% of their time developing new reports rather than on churning out the data, you know you have got it right!
Support in transforming analytics
Over the last year we have been working with two hospices that are breaking out of the analysis paralysis – St Gemma’s in Leeds and St Barnabas in Lincolnshire. It is noticeable that both are dealing with very similar challenges, with similar data, and similar ambition. They both understand their own data inside out, so the ask has been to support them on their journey rather than do it for them. And they know exactly what they want: How do we automate our reporting? How do we improve data quality? What does health equity look like? How do we measure our impact?
With the right foundation in place, hospices can transform their analytics from a necessary burden into a powerful tool that truly serves their mission—improving patient care, demonstrating impact, and securing the future of hospice services in an increasingly data-driven healthcare landscape.
Get in touch for an informal chat about how we can help you transform your analytics:
Analytics@HereWeAre.org.uk
Also of interest
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data rich, information poor: Why analytics matters to hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Data rich, information poor: Why analytics matters to hospices appeared first on Here.
]]>The post Rethinking Our Health: Why it matters appeared first on Here.
]]>Rethinking Our Health: Why it matters

Our CEO explores why rethinking health matters now more than ever and how community-powered approaches can reshape the future of healthcare.
The moment that sparked a quiet revolution
In the summer of 2022, we were deeply inspired by a document from New Local – A Community-Powered NHS co-authored by Adam Lent, Grace Pollard and Jessica Studdert. The principles of community powered health were a clarion call for Here, triggering a quiet revolution in how we delivered our services.
A series of conversations in our clinical teams led to a series of startling innovations across our services, that New Local helped us to take to a wider audience. Our Community Appointment Days approach pioneered in the spring of 2023 is now unquestionably one of our most impactful innovations in delivering healthcare services. More than 120 providers across the UK have now engaged with Community Appointment Days – either adopting the model or actively exploring how to replicate it, changing our expectations of where and how healthcare should be delivered. So, when Adam says what he has written now is the most important thing since then, it’s time for us to take a look.
A healthcare approach based on traditional telling, doing, treating needs a radical rethink
Doing with, not doing to
Doing With: Reinventing Public Services In A Time Of Crisis | The King’s Fund speaks clearly to the challenge of our time – and today we are already in lock step with the approach outlined. Since the earliest days of our services for people with long term conditions we have built in patient leadership. Our staff now known as ‘Health Builders’ are a critical part of our infrastructure – people with lived experience who design and deliver services with the community, enabling the ‘do with’ approach that is so critical to our wider public service reform.
Why healthcare needs a rethink
Nowhere is this more critical than in healthcare. Given 80% of the determinants of health are not related to access to healthcare, a healthcare approach based on traditional telling, doing, treating needs a radical rethink – particularly when it comes to the upstream shift to prevention set out in the ten-year plan. Now, compared to when the NHS was founded, 65% of NHS spending is on long term health conditions.

From treatment to management
What this means is the treatment paradigm needs to shift. For at least 65% of the time, we need to be focused on and enabling ‘management’ over treatment. That means a deep collaboration – led by the citizen, to understand how they want to manage their health condition and integrate this management approach into their daily life, to make sure they have the life that matters to them.
The language of healthcare: time for a rewrite
This frame does not feel shocking to me, and yet the implicit rules that underpin how we deliver healthcare suggest that this approach will be deeply radical. Nowhere is this more present than in the language we use to describe healthcare interactions. We ‘consult, prescribe, treat, review, discharge’. Patients ‘wait, present, comply, disengage or DNA’. We talk in acronyms and euphemisms, about CVD, COPD, CVA, about activation levels, health literacy, risk factors and the ‘hard to reach’.
We treat episodically, with little view of the whole person or their whole lifespan.
Listening with curiosity, humility, and a willingness to let go of assumptions is a radical act, one that can unlock different outcomes.
From patient to person
We ask if they are taking their prescribed medication daily, not if they are walking, talking to others, living in a place they can call home with good work, good friends and a good life.
Only rarely do we connect as humans, acknowledge what matters most, and work together to enable it to happen. Joy, connection, quality of life do not show up in our lists of key performance indicators or our measures of productivity.
Listening is a radical act
Part of what gets in the way is the rigorous training, expertise and experience that sits in the hands of our health professionals. With so much hard-won knowledge and skill, it is challenging to adopt a listening approach, to acknowledge that what we care so passionately about may be of secondary importance to the patient in the room.
Listening with curiosity, humility, and a willingness to let go of assumptions is a radical act, one that can unlock different outcomes.
Charting a new course, Rethinking Our Health project
We know a different approach can work. In the pockets around the country that Adam highlights, new types of conversations are happening, and communities are uniting with new purpose. We’re excited to be exploring how to ‘rethink our health’ in a project at Here. We hope to both design and test new ways of connecting healthcare to communities – to map how healthcare services best ‘dock’ to places and the people they serve is our primary focus.
Alongside this, we want to track how change happens, what makes it possible and sustainable, and to share our learning as widely as we can.
We’re still early in this journey, but we believe this is where the most important work lies, and we’re not alone.
If you’re rethinking health too, we’d love to connect.
We’ll be sharing our learning as the project develops – publishing regular reflections on what works and what doesn’t.
Sign up to updates direct to your inbox
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Rethinking Our Health: Why it matters appeared first on Here.
]]>The post Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust appeared first on Here.
]]>Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust

Reflections from our first Rethinking Our Health codesign workshops.
Codesign events with communities and partners
July saw an important milestone in Rethinking Our Health, with our test site partners we held community codesign events to share back the findings of the engagement phase, and to discuss practical ideas to take forward in the autumn. These will be focused on our goal of community-designed, clinically backed support for people with or at risk of osteo-arthritis, cardiovascular disease and diabetes.
A mix of lived and professional experience

At both events we had a half and half mixture of community members and people who work in health, local government, and the voluntary community and social enterprise (VCSE) sector.
Designing the events with the community
Both events were planned with our test site partners and community members, and this is key to how they went. This meant focusing on the biggest things people told us about in the engagement phase – there were pain, access to services, understanding and confidence around your condition, practical social and financial barriers.
Two areas, two approaches
In one test site there has been a history of (and a funded infrastructure for) conversations and partnership working. Over the last ten years, many issues have been discussed, the progress both desired and created by all, the codesign event felt natural. It felt like we could ask things of each other.
In our other area leadership is more dispersed, local government takes a bigger role in leading and encouraging community health and engagement partnership working. Test site partners took a participatory appraisal approach to developing community engagement in our big question, and the pre-event work was important to building interest and confidence to take part.
Shared energy and commitment
One thing in common was that both events were buzzing with enthusiasm and commitment to neighbourhoods was clear. There is a real appetite for building on existing or previous work, ambition for better solutions and understanding that so much of this is built on relationships.

What we heard: Key themes from the codesigns
Key themes that came out of both events were
- desire for local, early, holistic support
- positive and ambitious views on the role of community and VCSE in this
- community engagement and mobilisation, patient leadership and voice is critical
- importance of being heard, and *feeling* heard – both in individual situations as well as a community
We heard a range of views about what kind of support could be given by clinicians versus non-clinicians, and creating different configurations of how community and clinician support could be offered together.
Clinical risk and collaboration
There’s an important discussion to be had about understanding and managing any clinical risk, which Here as a clinical and community-rooted organisation is well-placed to host.
Looking ahead

This way of working is how health care will be developed over the next ten years and beyond.
Dr Rowan

For now, sign up to receive an update when we publish the next blog. Want to get in touch about Rethinking Our Health? Email us: Collab@HereWeAre.org
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Pain: Insights from The Kings Fund and Here
What if pain wasn’t just something to manage, but a signal for change? The Kings Fund and Here explore how a “do with” approach can transform pain services – focusing on prevention, connection, and holistic support.
The post Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust appeared first on Here.
]]>The post Here shortlisted for HSJ Award 2025 for CADs appeared first on Here.
]]>Here shortlisted for HSJ Award 2025 for CADs

We’re delighted to share that Community Appointments Days (CADs), developed by Here as part of Sussex MSK Partnership has been shortlisted for a 2025 HSJ Award in the Primary and Community Care Innovation of the Year category.
This shortlisting is a celebration of the collaborative effort that brought CADs to life – including our brilliant partners at Sussex Community NHS Foundation Trust, local VCSE organisations, and the dedicated clinicians, care navigators and volunteers who are reimagining care with us.

Community Appointment Days (CADs)
Our entry showcases the innovative CAD model of care co-designed with patients, clinicians and voluntary sector partners. CADs are transforming how people experience MSK (musculoskeletal) support by bringing together whole teams of professionals in local community spaces, and delivering same-day, person-centred care shaped around individual priorities.
“What could have taken a few months was made possible in 1.5 hours.”
— Patient feedback from a CAD
The CAD vision
Born from a vision to take care out of hospitals and into the heart of communities, CADs enable people to get the support they need in one visit – from clinical advice and self-management plans to wellbeing coaching and social prescribing. With over half of attendees discharged to self-care on the day, and outstanding feedback from both patients and staff, CADs are delivering real impact – and a powerful example of what becomes possible when we start with trust, partnership, and the question “What matters to you?”
Shortlisted from over 1,250 entries nationwide
The most coveted accolade in UK healthcare, the HSJ Awards is the largest annual benchmarking and recognition programme for the health sector. This year’s awards attracted more than 1,250 entries from across the health sector. With only 245 projects and individuals making it through to the final shortlist, the competition has been incredibly tough, demonstrating the impressive scale of talent, commitment, and impact across the NHS and wider healthcare landscape.

Our shortlisted entry for Community Appointment Days, was selected following a rigorous judging process and has been recognised as a standout example of excellence in healthcare delivery.

We are honoured to be shortlisted for the HSJ 2025, Primary and Community Care Innovation of the Year award. This recognition is a testament to what’s possible when we put people at the centre of care and work across traditional boundaries. Community Appointment Days are built on trust, collaboration and listening – and they’re making a real difference to people’s lives. I’m incredibly proud of the teams and partners who have made this happen and delighted to see their work acknowledged on a national stage. To be recognised among so many outstanding initiatives is already a win in itself.
Helen Curr
CEO at
Here

HSJ Editor Alastair McLellan commented: “On behalf of all my colleagues, it gives me great pleasure to congratulate Here on being shortlisted as a finalist in the category of Primary and Community Care Innovation of the Year. All of the applications represent the ‘very best of the NHS’ and often leave our esteemed panel of judges with an impossible choice! Year on year the number of entrants continue to rise which I find so encouraging and is testament to the effect that HSJ Awards can have on improved staff culture and morale.”
We’re proud to stand alongside others who are pushing boundaries and demonstrating that integrated, person-centred care is not just possible, but essential for the future of healthcare.
Thank you to everyone involved and congratulations to all the other inspiring projects and teams shortlisted this year!
Also of interest
Early Pain Support: Insights From our first Community Drop-In
As part of Rethinking Our Health, we hosted our first community pain drop-in — a chance for people to talk things through early, get reassurance, and feel more confident about managing pain. This blog shares what we learned, and why having the right conversation at the right time really matters.
New RCGP Report Highlights Hidden GP Workload
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
Data and Analytics: why we work with hospices
Like many of us delivering healthcare in collaboration with the NHS, hospices are experiencing the dilemma of not being an NHS organisation but needing to know our way around the landscape of data as if they are.
The post Here shortlisted for HSJ Award 2025 for CADs appeared first on Here.
]]>




