From health inequalities to creating health equity

“By creating a mission around health equity, we can connect our staff to a bolder vision for their work, with healthcare workers as agents of social change, making a difference to our world rather than processing an endless chain of individuals passing through.”
In 1834 Britain passed the Poor Law, an act of Parliament partially creating a safety net for all, but also enshrining a principle of deterring people from making unnecessary demands on public funds that remains present in today’s national debate.
The infirmaries that grew from the poor house would soon be described as “a disgrace to our civilisation” (Lancet 1865) and served as inspiration for the alternative visions of Beveridge and Bevan a generation on.
The Marmot review in 2010 and ten years on (2020), along with the desperately disproportionate impact of COVID show how slow our progress has been.
Poverty continues to kill people in Britain, whether through poor housing (Awaab Ishak: Rochdale housing boss admits 1,800 homes have mould – BBC News), starvation (Disabled man starved to death after DWP stopped his benefits | Disability | The Guardian) or the wider impact of poverty on diet and obesity (Food insecurity as a risk factor for obesity: A review – PMC (nih.gov)) and mental health (Briefing 58: Poverty, economic inequality and mental health – Centre for Mental Health).

Health inequalities today
In today’s Britain, healthy life expectancy remains widely divided between rich and poor with inequities widening since 2010 English indices of deprivation 2019 – GOV.UK
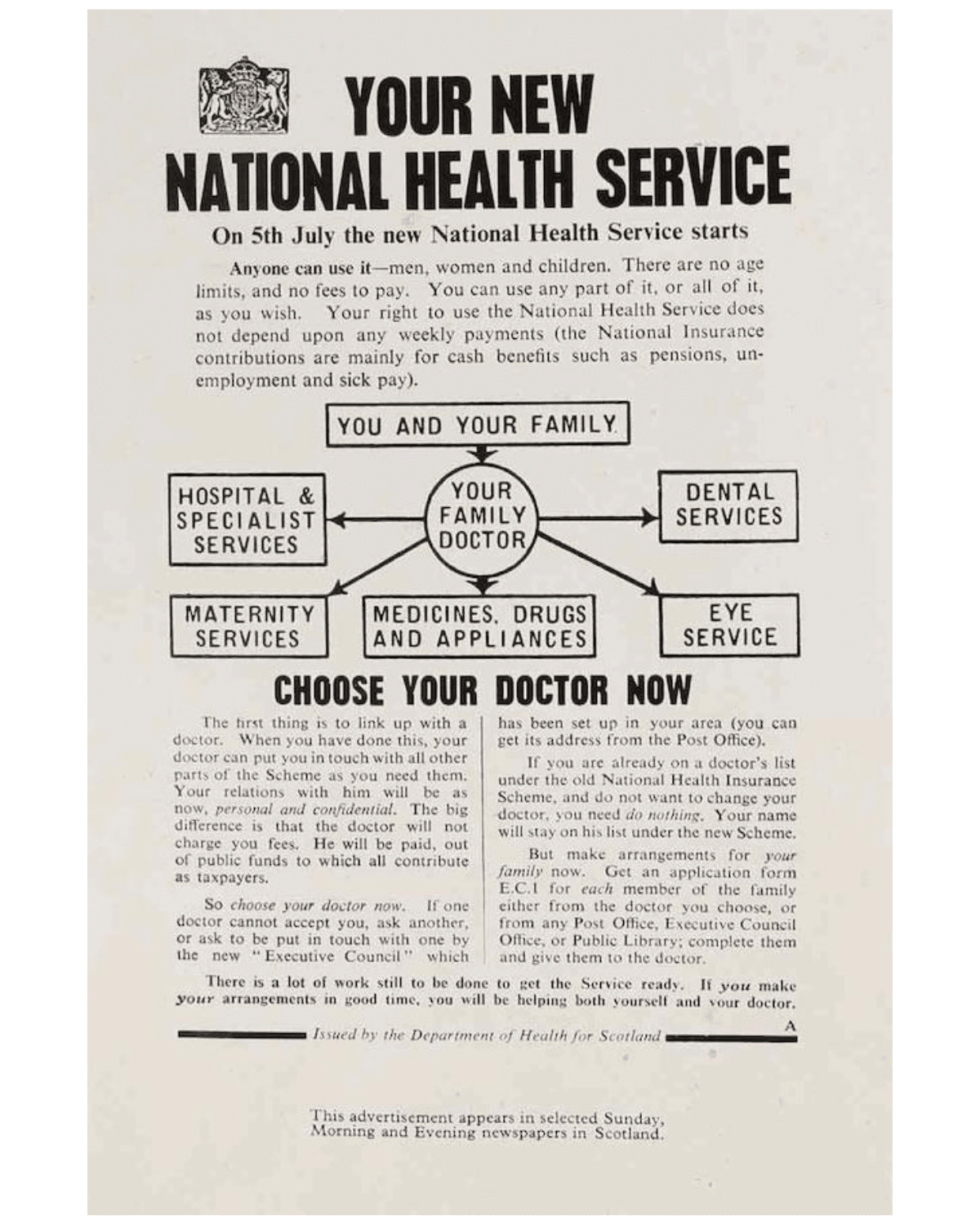
Nye Bevan’s vision for the NHS was a far-reaching reform of access to healthcare, with a more dramatically socialist root than is widely spoken of.
In providing universal access to healthcare, free at the point of delivery, Bevan viewed the NHS as part of an infrastructure that would dismantle division of class and wealth.
When we talk about health inequalities today, we often think of correcting poorer health outcomes, and less about social justice.
There is a risk that we fail to recognise in real terms the need to deliver more (and different) health and social care interventions for some people, rather than just making sure there is equal access to the traditional offer.
Shifting the language from health inequalities to creating health equity
More insidiously, at times of high demand, services can pivot to the quick wins, trying to reduce overall waits or meet blunt targets. At these times, delivering care to groups with different needs can feel more challenging, ‘complex’, and bypassed on route to the ‘low hanging fruit’.
During the rollout of the COVID-19 vaccine, we saw this in real time, with data tracking how some populations accessed vaccine quicker than others, and the cost of delivering to some groups was higher – and therefore not incentivised in a fixed tariff payment mechanism.

Wider than this, we know the presence of health conditions or caring responsibilities adds disadvantage over time, a vicious cycle where 54% of carers report their own health had suffered, and 44% had put off seeking health treatment because of their responsibilities. For these groups ‘equal’ access to treatment as usual will not meet their need.
Shifting the language from health inequalities to creating health equity paints a much broader picture.
It engages our services in recognising that part of the mission of the NHS is a social justice one, that we are a part of how wealth is re-distributed, by providing safe, universal, free access to healthcare, we can balance the accident of birth. As Marmot says, “if health has stopped improving, it is a sign that society has stopped improving”.
Healthcare workers agents of social change
By creating a mission around health equity, we can connect our staff to a bolder vision for their work, with healthcare workers as agents of social change, making a difference to our world rather than processing an endless chain of individuals passing through.
From this lens, we are stretched to consider what more we can do, taking proactive approaches to the delivery of health, seeking out places and populations who we know are disadvantaged, and playing our part in levelling the playing field.
With this focus, our task is shaped differently. No longer do we look at access data in terms of whether it is representative of our population, but whether it is representative of our population need.

Our programs and services spend more in areas of deprivation, understand that delivery methods than may be more expensive, and focus on the value this represents in lifting the disproportionate distribution of wealth (in its widest sense).
Doing things differently for a better world
More contentiously it could mean sifting through these long waiting lists differently – to identify those who are disproportionately impacted, less advantaged, less resilient, less able to wait, in service of a fairer society.
It is as much part of our social mission as it is our commissioned services, and we want to do more. We are not alone. Despite all of the pressures within the NHS, we know there is a growing emphasis and commitment to the pursuit of a better world, a drive for health equity at every stage of our lives.
Through our data dashboards and outreach programs (Vax and CAD), we have learned about how to deliver healthcare differently. Delivering quick, efficient healthcare to the many, and bespoke, targeted offers to the few.

We believe we’re stronger together. If you’d like to work with us to find new and innovative ways of growing health equity then we would love to hear from you.
Get in touch: collab@hereweare.org.uk
Dr. Helen Curr, Chief Executive at Here
My role is to hold ourselves true to our values. To make sure our commitment to putting people at the heart of their healthcare journey is embedded in every decision and action we take.

Also of interest
Rethinking Our Health: starting with pain
We’ve been asking communities what really matters when they’re living with pain. In this update, we share what we heard, what surprised us, and how this learning is shaping a new three-part support offer for MSK pain that starts locally, builds on existing strengths, and is designed together.
Rethinking Our Health: Why it matters
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.
Ingredients for community codesign: a venue, some flipcharts, a bowl of soup and a lot of trust
Introducing Rethinking Our Health – a new way of working with communities to support people living with long-term conditions.


