Case study
Transforming stroke patient pathways
Funded by NHS England’s SQuIRe catalyst programme
The Stroke Health and Wellbeing Service Pilot: What we set out to do
We started this project with the aim to transform stroke care in Sussex by offering better support for stroke survivors and their loved ones. Through a strong, personalised and integrated community stroke service.
From January 2023 – March 2024, we tested a series of innovations in Brighton & Hove and High Weald, Lewes and Havens.
Working closely with our partners and cruicially also people with lived experience of stroke we explored what was needed to help support people, developed big ideas and created a plan for how stroke services could be improved nationally.

The big ideas
Some key models informed the project

The ISDN 6 Pillars informed the aims for the project:
1: Centering “What matters”
People experience personalised, integrated care focused on their needs, while addressing health inequalities.
2: Using lived experience
Personalising care by Health Builders who know stroke recovery.
3: Opening access
People can get support and care 7 days a week, regardless of who they are or where they live.
4: Creating a sustainable model
Building a sustainable and replicable model with sharing of learning at its heart.
5: Innovating workforce solutions
Reviewing skill mix and the use of Non-Clinical Healthcare Professionals.
6: Finding a new workforce
Scoping using a novel workforce, including student placements, voluntary sector and domiciliary care.

92% of people seen in the service said:
“I felt supported to get back to my hobbies and interests”

How the Stroke Health and Wellbeing project worked in 5 stories
1: Effective use of resources
Creating new support roles in Health Builders and Stroke Support Workers, and offering proactive support has made a measurable difference to people’s care experience and outcomes (see appendices iii and iv), regardless of background (see appendix v).
2: Improving staff experience
The service’s person-centred and proactive support has also created a positive impact for staff. Stroke Support Workers have scope and space to tailor care to individuals, leading to better outcomes and meaningful work (see appendices i and ii for role scope and activity).
3: Saving clinician time
The support Health Builders and Stroke Support Workers have been able to offer stroke survivors and their loved ones has freed up clinicians to do the work only they can. This has saved clinical time at the same time as improving experience and better meeting care needs.
4: Living with purpose
The work of Health Builders has made a huge difference for those they have helped, and also for the Health Builders themselves. The role has provided a way to give something back, to return to working life, to be part of a team – supporting living with purpose which is important in the ongoing journey of recovery.
5: Speeding up recovery
People seen in the service have reported quicker recovery and an outstanding experience. Practical support and lived experience have translated into improved motivation in recovery and attaining personal wellness goals (see appendix iv).
Lessons learned and what next?
System change needs energy
Introducing new ways of working into a system which multiple demands and pressures is challenging. Band width and readiness to experiment is variable and change fatigue is part of the context that our healthcare system is operating in.
As a pilot project, this project had to move swiftly and keeping our momentum was helped by focusing efforts where teams were most able to engage and collaborate. For example, appetite for peer support sessions at Royal Sussex County Hospital led to the development and expansion of the Health Builder role and input.

To move at speed
We had 15 months to mobilise, deliver and evaluate the service.
Making and then acting on decisions at speed was helped by listening to our principles of personalisation, data and trusting people, rather than being too rigid in our approach.
Devolving responsibility quickly by offering structured support and trusting Health Builders to use their expertise well made a huge difference.
Ensuring we took care up front to set benchmark measures that would show the impact of the work paid off later.


Proving cost value
The service saw people for 9 months. There was strong evidence of good outcomes and strong anecdotal evidence of saved clinical time, but further time and research is required to understand financial impact:
- Tracking 62 people to compare this cohort’s outcomes with previous records or a control group
- Following up anecdotal evidence of saved clinical time at hospitals
- Exploring the impact of further stroke prevention and cost impact of this
Ensuring we took care up front to set benchmark measures that would show the impact of the work paid off later.
People want to help
An unexpected realisation was how much those who have been helped in stroke recovery are motivated to help others.
The support of Health Builders and Stroke Support Workers had a huge impact on stroke survivors and their loved ones. Some of these people in turn are keen to offer their support to those earlier on in recovery.
Trusting and enabling people to offer their energy is a valuable resource ripe for exploration.
Integration hits limits
Catalyst funding has enabled the project to learn how to create a sustainable and integrated stroke support service.
Although we have successfully joined up expertise and learning, we have seen how siloed financial resources limit the extent to which the service can be truly integrated.
Exploring joint commissioning and collaborations that pool resources between trusts and organisations is part of the necessary structural change required to underpin lasting impact and change.

Unlocking data flow
In acute setting scenarios where data was coded on paper, we requested access and coded them into a bespoke SystmOne unit. We engaged with local system tech workstreams such as Plexus to gain sight of patient data. A lack of sufficient detail in the acute and community settings was mitigated by the community services using SystmOne, allowing for record sharing. We also considered the Sussex Integrated Dataset project.
Integrating SystmOne with Azure Datawarehouse and Power BI provided an excellent solution for near real-time data flow for timely analysis.
We’re not alone
It has been continually encouraging to discover that we are not alone in what we are learning works to build effective services that deliver better better health outcomes.
ICSS, ILASS, IPCAS, the Major Conditions Strategy, PICAS – these strategies mirror the findings and intentions this project has put into action.
We who do this work can feel confident we are part of a wider movement towards community powered personalised care and population health.

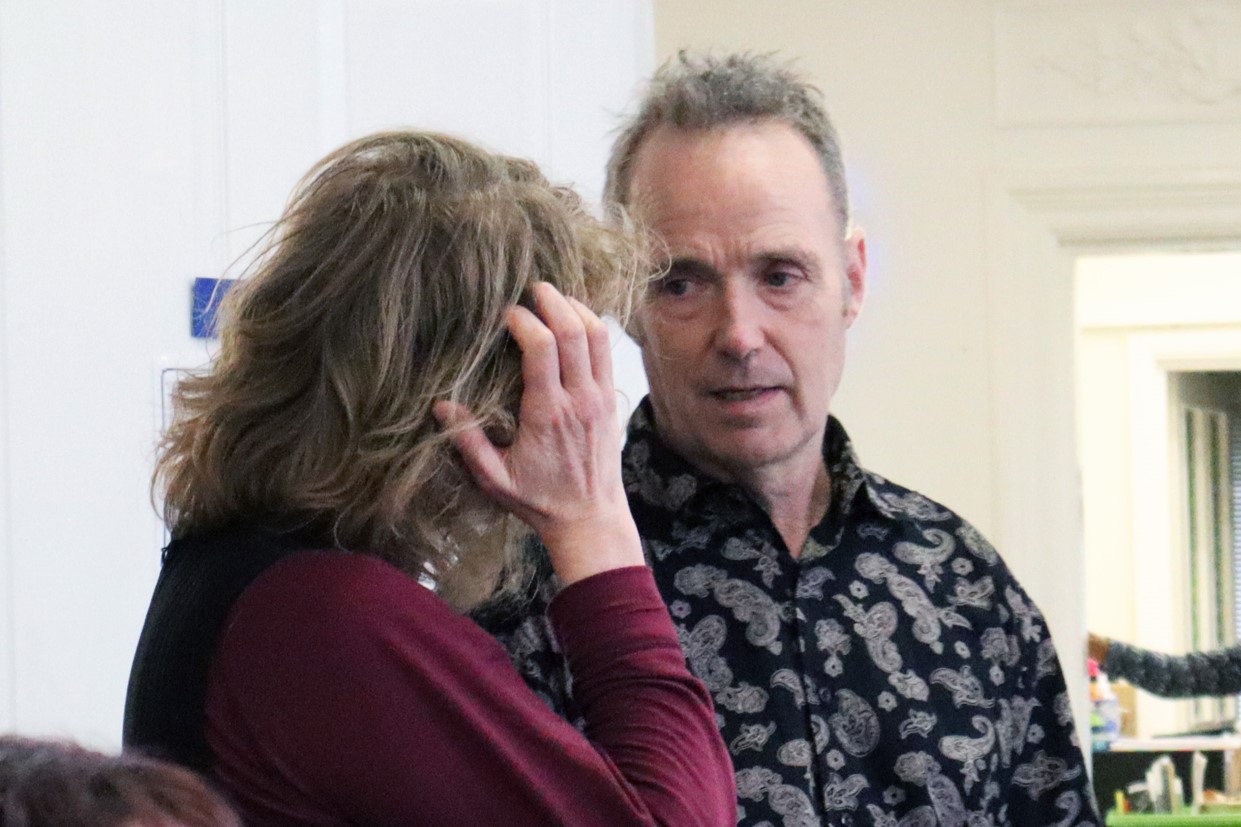
From the very start, Health Builders have been equal partners in our planning workshops and a key part of the decision-making process… It has been inspiring to witness the Health Builders in action, as they have grown in confidence and purpose themselves. The value of their efforts in supporting fellow stroke survivors to live their best life is immeasurable.
Norman Webster
Lead Health Builder at Here

If you’d like to discuss working together with us we’d love to hear from you.
Email: collab@hereweare.org.uk
How else we can help
Health services delivery: We design and deliver CQC ‘Outstanding’ services and pathways.
Tools and training for health professionals: We provide award-winning analysis, automation tools, and time-saving training.
Healthcare innovation: We develop bold solutions to transform long-term conditions services and pathways.