Stroke: Cardiovascular disease
Transforming stroke care pathway in Sussex
Service: HSE SQUIRE funded Catalyst Quality Improvement Project
Partners: NHS Sussex, Sussex Community NHS Foundation Trust, University Hospitals Sussex NHS Foundation Trust, NHS England, Stroke Association, Headway Sussex
Reach: Brighton & Hove and High Weald, Lewes and Havens
Impact of our transformed stroke service
Our stroke and wellbeing service transformation brought people with lived experience together with health professionals from across Sussex to support those who have been affected by stroke.
Together we designed rehabilitation care, personalised to each person and shaped around what matters most to them.
- People have access to the support and care they need 7 days a week, regardless of who they are or where they live.
- People experience a truly integrated and personalised care journey that puts ‘what matters to you’ front and centre of their care.
- The model is sustainable, replicable and proactively addresses health inequalities.
Stroke transformation impact
felt supported in returning to hobbies/activities that mattered to them.
45% higher than the Sussex PREM survey 2023
reported improvement or maintenance in activation.
achieved all their ‘what matters most’ goals
(mental health, mobility, pain management, personal care and usual activities)
The transformed Sussex Stroke and Wellbeing Service provides:
- A single point of contact for patients and carers. Patients are allocated a named stroke support worker (SSW) in acute settings who will support people on their journey with Stroke both in acute and onwards into community settings.
- ‘What Matters to You’ conversations, meeting needs through care navigation and social prescribing, focusing on recovery and living well.
- Bespoke, responsive and personalised needs-based support as well as structured support that includes First Contact, 3 Month and 6 Month follow-up. All information is shared electronically with primary care and community teams as appropriate.


How we transform stroke and well-being services
Our approach to improving stroke services in Sussex started with three innovative and complimentary transformation packages.
Designing out health inequality
This matters because:
“People in inclusion health groups tend to have poor experiences of healthcare services because of barriers created by service design. These negative experiences can lead to people in inclusion health groups avoiding future contact with NHS services and being least likely to receive healthcare despite have high needs.
This can result in significantly poorer health outcomes and earlier death among people in inclusion health groups compared with the general population.”
https://www.england.nhs.uk/long-read/a-national-framework-for-nhs-action-on-inclusion-health/
We were able to mitigate the usual effects of social and demographic factors on access, experience and outcomes of care by creating a truly integrated and personalised service. Everyone received personalised support while in the hospital, and the care provided was tailored to their individual needs and preferences, as well as those of their loved ones.
This is in stark contrast to the negative patient experiences referred to in The National Framework for NHS Action on Inclusion Health, when the way healthcare services are organised, accessed, and delivered can amplify health inequality rather than address it.
Our transformation model
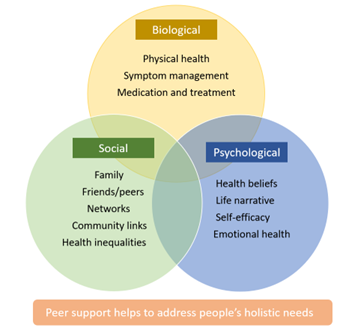
We understand that when a life-changing event like a stroke occurs, people require personalised, holistic care to aid their recovery and assist them in rebuilding their lives. This means addressing the multiplicity of needs people have, but stroke services traditionally centre on biological and medical needs alone.
We introduced a model based on the biopsychosocial model of care that complements the existing stroke services and provides stroke survivors and their carers with a three-pronged support system.
- Clinical care
- A named stroke support worker offering personalised support with whatever the person or their carer needed
- Peer support groups with people with lived experience
Crucial to the new system is the Stroke Support Worker. They are a single point of access for stroke survivors, helping them navigate holistic care and personalise clinical pathways.
If you’d like to discuss working together with us we’d love to hear from you.
Email: collab@hereweare.org.uk